
Patella instability in the skeletally immature patient: pearls for surgical treatment
Introduction
The management of patella instability in children and youth is problematic with a recurrence rate of patella dislocation following non-operative treatment reported to be from 15 to 80 percent and on average, 40 percent (1). The reason for this high failure rate is no doubt multifactorial, in part due to the lack of scientific validation of non-operative treatment regimens and in part due to the presence of pathoanatomies that predispose to patella instability (2). These pathoanatomies include trochlear dysplasia, patella alta, increased knee valgus, increased Q-angle and increased tibial tuberosity:trochlear groove distance (TT:TG distance). Other features that create susceptibility to patella instability in children include hyperelasticity and torsional abnormalities of the lower extremity.
With such a high failure rate of non-operative management, surgical alignments and reconstructions are frequently required. When designing a surgical approach for the treatment of patella instability, the ideal process should address the “correction” of the underlying pathoanatomies that have been shown to be associated with the instability. In the skeletally immature patient, this can present a problem due to the presence of open growth plates (physes) since osteotomies can result in premature growth arrest and progressive deformity. For example, trochlear dysplasia has been shown to be commonly associated with failure of surgical treatment and one that cannot be addressed with osteotomy without the risk of growth plate injury (3,4). Therefore, when designing a surgical approach the risk versus benefit should be understood not only by the surgeon, but also by the parents and child as well.
The following discussion of “pearls” for the surgical management of patella instability is based upon the available literature as well as the experience of the author.
It is all about balance
When addressing patella instability surgically, it is all about restoring the balance of the extensor mechanism of the knee (5). This balance includes the static structures of ligaments and retinaculum as well as the dynamic myotendinous structures. With this approach we need to remember that competence of both medial and lateral retinaculum are required. Although we may visualize the retinacular restraints as coming from the medial/lateral coronal plane, they are actually more oriented closer to the sagital plane with a function to guide and settle the patella into the trochlear groove, from which the slope of the lateral wall of the trochlea has been shown to then become the primary restraint to lateral patella displacement (6).
Too loose is better than too tight
Patients with patella instability present in two types; those with instability and patellofemoral malalignment (patella subluxation and even dislocation) and those with instability but with normal patellofemoral alignment relative to the trochlear sulcus. In either case, the objective of the operation is to prevent further dislocations and that will include a medial repair and/or reconstruction. Although the temptation for medial repair/reconstruction is to follow a (false) principle that “tighter is better,” that temptation only leads to over-constraint with potential complications of stiffness, pain, and patellofemoral arthrosis (7). Therefore when repairing and/or reconstructing the medial side, insure that the normal medial/lateral patella translation of two quadrants of patella glide is restored. Too tight is definitely not better than too loose.
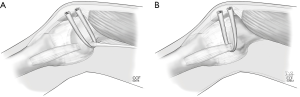
Don’t give up on the medial retinaculum
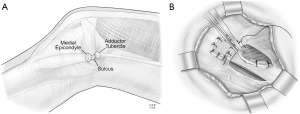
A tendon reconstruction of the medial patellofemoral ligament (MPFL) has become a generally accepted component of the surgical treatment for patella instability and for good reason. However, it is technically demanding and associated with potentially devastating complications such as knee stiffness, pain, and patellofemoral arthrosis (7). That said, if the patient does not have trochlear dysplasia and does not have hyper-elasticity and does not have patella alta, a proximal patella alignment to include imbrication of the medial retinaculum (and lateral retinacular lengthening as needed) can be very effective with much less potential for post-operative complications (8). Remember that the normal state of patellofemoral equilibrium only requires the competence of a very thin and relatively weak retinaculum (Figure 1).
Don’t wait until growth plate maturity
Although the surgical treatment of patella instability in children is problematic, the benefits of creating realignment of the patellofemoral joint outweigh the risks. Namely, the development of a competent immature trochlea is dependent upon the presence of patella contact. Leaving significant patella subluxation (patellofemoral malalignment) along the developing distal femur can be associated with trochlear dysplasia. The flip-side of this is that restoration of normal patellofemoral alignment in the very young (pre-pubescent) child can have the potential of restoring normal trochlear development. Perhaps a “softer” justification of proceeding with surgical intervention in the skeletally immature patient is the pure disability and morbidity that is associated with episodes of patella dislocation as well as the potential for chondral injury.
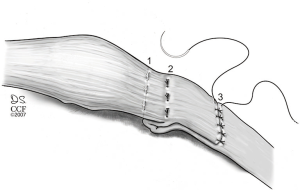
Lateral lengthening rather than lateral release
As noted above, the balance of the extensor mechanism of the knee and stability of the patella is dependent upon a functioning medial and lateral retinaculum. Although the primary soft tissue restraint to lateral patellar displacement is the MPFL (located within the intermediate layer of the medial retinaculum) (9,10), the lateral retinaculum (primarily the deep transverse lateral retinaculum) provides 10–15% of the soft tissue restraint to lateral translation (11). Furthermore, the primary cause of medial patella subluxation/dislocation (medial instability) is post-lateral retinacular release. When first recognized as the painful disabling condition that it is, the primary cause was found to be an excessive lateral release that was carried well proximal into the tendon of the vastus lateralis (12). The only true indication for a lateral retinacular release is refractory anterior knee pain associated with a tight lateral retinaculum. And even then, it is probably best to lengthen the lateral retinaculum rather than release (Figure 2).
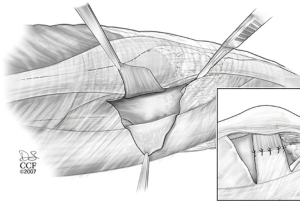
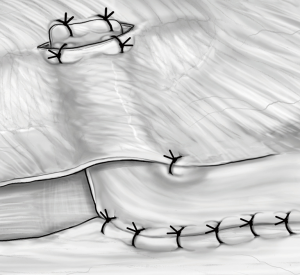
When dealing with patella instability in the hyper-elastic patient, part of the proximal soft tissue alignment and reconstruction can often be aided by the addition of a lateral reconstruction (not release or lengthening) as well as medial reconstruction (Figure 3).
Medial patellofemoral ligament reconstruction (MPFL-R)
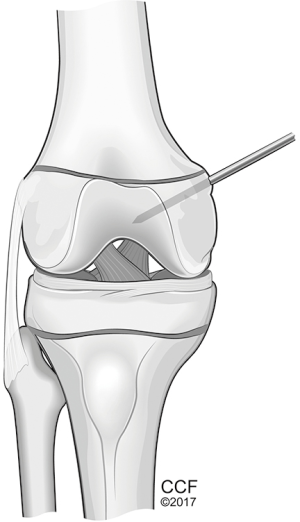
Perhaps one of the most important surgical techniques developed for the management of recurrent lateral patella dislocations has been the reconstruction of the MPFL (13,14). Although described decades ago, it has been over the past decade that a better understanding of the anatomy and biomechanics has been provided (15). Although there are various interpretations of the origins and insertions, most commonly it is felt that the transverse fibers of the MPFL originate from a sulcus located between the adductor tubercle and the medial femoral epicondyle and insert into the proximal half of the medial boarder of the patella (9). More recently, Fulkerson has illustrated the additional fibers that blend with the quadriceps tendon (16). Baldwin has also described oblique fibers that blend into the anterior boarder of the superficial medial collateral ligament (9). That said, for most the attachment of a tendonous reconstruction (typically using either semitendinosus or gracilis or quadriceps tendon autograft; or similar allografts) will be docked at this sulcus. Whether adult or child, when reconstructing the MPFL, avoid transverse drill holes across the patella for fear of subsequent stress fracture and test for “isometry” prior to final fixation. Too loose is better than too tight and allow for a normal amount of patella stability with two quadrants of patella translation.
The issue in the skeletally immature patient is the distal femoral growth plate. This physis is not linear. It undulates and has a convex distal orientation. Therefore, if a drill hole to be used for a docking type of femoral fixation is used, the orientation should be directed slightly distal and not transverse for fear of violating the physis (17) (Figure 4). Furthermore, Farrow has also advocated that the direction should not only be directed distally but also anteriorly to avoid physis injury. Finally, two other techniques for femoral fixation have been described for the skeletally immature patient in order to avoid the growth plate (18,19) (Figure 5A,B). A free tendon graft can be anchored around the tendon of the adductor magnus adjacent to the adductor tubercle; or the graft can be passed around the superficial medial collateral ligament adjacent to the medial femoral epicondyle. When using these variations of attachment, it is critically important to understand the strain patterns of the graft. When using the medial collateral ligament as an attachment site it will result in greater length (and strain) required in extension and lessening strain in flexion. Therefore as the final fixation is applied to the patella, the knee should be in full extension with proximal traction applied to the central quadriceps tendon (simulating quadriceps contraction). The flip-side of this is when the tendon of the adductor magnus is used as the femoral anchor. Those that use this method will perform the final fixation with the knee in 45–60 degrees of flexion in order not to over-constrain the knee as it goes into flexion. In either case, as emphasized before, too loose is better than too tight.
Patella alta
A frequent pathoanatomy associated with recurrent patella dislocations in children and youth is patella alta. There are several problems with this diagnosis, one of which is deciding how to define it in the first place. Radiographic indices such as the Insall-Salvati Index, the modified Insall-Salvati Index, the Blackburne-Peel Ratio and the Caton-Deschamps Index have been well documented with the latter being judged to be the most consistent (20). However, since plain radiography only illustrates the bony anatomy and not cartilage, Biedert has described a method using Magnetic Resonance Imaging (Patella-Trochlea Index) (21). However it is determined, a patella that rests too far proximal to the trochlea with the knee in extension is a risk factor for dislocation. In the adult this pathoanatomy can be addressed by tibial tuberosity osteotomy with distalization. In the child, this is not an option due to the open apophysis of the tuberosity. However, methods of patella tendon shortening have been described and modified by Andrish, which can be applied to the child as well as the adult (22) (Figure 6).
Trochlea dysplasia
This pathoanatomy is one of the most common associations with patella instability and the most common condition linked to failure of surgical intervention (3). In the adult, various methods of trochleoplasty have been described with documented efficacy. In the skeletally immature patient, however, osteotomy is risky and for most, avoided. The addition of MPFL reconstruction, however, has been a significant help for the treatment of these individuals, especially in the more common mild forms of dysplasia (14,23).
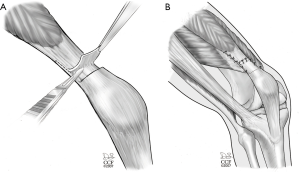
Congenital fixed lateral patella dislocation/obligatory patella dislocation in flexion
Much less common are the fixed lateral patella dislocations as well as those that dislocate every time the knee flexes. In those conditions there is most often an associated contracture of the quadriceps. Although the alignment of the extensor mechanism can be achieved by appropriate lateral releases and lengthenings followed by medial imbrications and reconstructions, in order to maintain alignment while achieving adequate flexion, a lengthening of the quadriceps tendon is required (Figure 7). Without including a quadriceps lengthening, one of two complications can occur. The first is a permanent restriction of flexion while maintaining patellofemoral alignment. The second possibility is that adequate flexion is achieved during the rehabilitation process, but at the expense of the loss of patella stability with recurrent obligatory lateral patella dislocation as the knee flexes (22).
Summary
The management of patella instability in children and youth can be challenging due to the presence of open growth plates that prevent the use of osteotomies of the tibial tuberosity and trochlea. Furthermore, reconstructions of the MPFL have the potential to violate the distal femoral physis, leading to premature closure and subsequent angular deformity. That said, most often surgical techniques are available to address these issues and lead to the safe establishment of balance and stability of the extensor mechanism of the knee necessary for improving the quality of life in the young patient. There is no need to delay surgery until skeletal maturity. For those seeking the latest consensus on the management of patella instability, a recent on-line publication is available (13).
Acknowledgments
I would like to acknowledge the editorial assistance by Nipun Sodhi in the preparation of this manuscript as well as David Schumick (Department of Medical Illustrations, Cleveland Clinic) for the preparation of the medical illustrations.
Funding: None.
Footnote
Provenance and Peer Review: This article was commissioned by the Guest Editors (Vicente Sanchis-Alfonso and Scott F. Dye) for the series “The Patellofemoral Joint” published in Annals of Joint. The article has undergone external peer review.
Conflicts of Interest: The author has completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/aoj.2018.04.04). The series “The Patellofemoral Joint” was commissioned by the editorial office without any funding or sponsorship. The author has no other conflicts of interest to declare.
Ethical Statement: The author is accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Fithian DC, Paxton EW, Stone ML, et al. Epidemiology and natural history of acute patellar dislocation. Am J Sports Med 2004;32:1114-21. [Crossref] [PubMed]
- Balcarek P, Jung K, Ammon J, et al. Anatomy of lateral patellar instability: trochlear dysplasia and tibial tubercle-trochlear groove distance is more pronounced in women who dislocate the patella. Am J Sports Med 2010;38:2320-7. [Crossref] [PubMed]
- Kita K, Tanaka Y, Toritsuka Y, et al. Factors Affecting the Outcomes of Double-Bundle Medial Patellofemoral Ligament Reconstruction for Recurrent Patellar Dislocations Evaluated by Multivariate Analysis. Am J Sports Med 2015;43:2988-96. [Crossref] [PubMed]
- Arendt EA, Donell ST, Sillanpää PJ, et al. The management of lateral patellar dislocation: state of the art. Journal of ISAKOS: Joint Disorders & Orthopaedic Sports Medicine 2017;2:205-12. [Crossref]
- Andrish JT. Recurrent Patellar Dislocation. In: Fulkerson JP. editor. Common Patellofemoral Problems, 1st Edition. Rosemont, IL: American Academy of Orthopaedic Surgeons, 2005.
- Farahmand F, Tahmasbi MN, Amis AA. Lateral force-displacement behaviour of the human patella and its variation with knee flexion--a biomechanical study in vitro. J Biomech 1998;31:1147-52. [Crossref] [PubMed]
- Bollier M, Fulkerson J, Cosgarea A, et al. Technical failure of medial patellofemoral ligament reconstruction. Arthroscopy 2011;27:1153-9. [Crossref] [PubMed]
- Cerciello S, Lustig S, Costanzo G, et al. Medial retinaculum reefing for the treatment for patellar instability. Knee Surg Sports Traumatol Arthrosc 2014;22:2505-12. [Crossref] [PubMed]
- Baldwin JL. The anatomy of the medial patellofemoral ligament. Am J Sports Med 2009;37:2355-61. [Crossref] [PubMed]
- Kruckeberg BM, Chahla J, Moatshe G, et al. Quantitative and Qualitative Analysis of the Medial Patellar Ligaments: An Anatomic and Radiographic Study. Am J Sports Med 2018;46:153-62. [Crossref] [PubMed]
- Merican AM, Kondo E, Amis AA. The effect on patellofemoral joint stability of selective cutting of lateral retinacular and capsular structures. J Biomech 2009;42:291-6. [Crossref] [PubMed]
- Hughston JC, Deese M. Medial subluxation of the patella as a complication of lateral retinacular release. Am J Sports Med 1988;16:383-8. [Crossref] [PubMed]
- Post WR, Fithian DC. Patellofemoral Instability: A Consensus Statement From the AOSSM/PFF Patellofemoral Instability Workshop. Orthop J Sports Med 2018;6:2325967117750352 [Crossref] [PubMed]
- Tompkins MA, Arendt EA. Patellar instability factors in isolated medial patellofemoral ligament reconstructions--what does the literature tell us? A systematic review. Am J Sports Med 2015;43:2318-27. [Crossref] [PubMed]
- Yoo YS, Chang HG, Seo YJ, et al. Changes in the length of the medial patellofemoral ligament: an in vivo analysis using 3-dimensional computed tomography. Am J Sports Med 2012;40:2142-8. [Crossref] [PubMed]
- Fulkerson JP, Edgar C. Medial quadriceps tendon-femoral ligament: surgical anatomy and reconstruction technique to prevent patella instability. Arthrosc Tech 2013;2:e125-8. [Crossref] [PubMed]
- Nguyen CV, Farrow LD, Liu RW, et al. Safe Drilling Paths in the Distal Femoral Epiphysis for Pediatric Medial Patellofemoral Ligament Reconstruction. Am J Sports Med 2017;45:1085-9. [Crossref] [PubMed]
- Andrish J. Surgical Options for Patellar Stabilization in the Skeletally Immature Patient. Sports Med Arthrosc 2017;25:100-4. [Crossref] [PubMed]
- Jacobi M, Reischl N, Bergmann M, et al. Reconstruction of the medial patellofemoral ligament using the adductor magnus tendon: an anatomic study. Arthroscopy 2012;28:105-9. [Crossref] [PubMed]
- Portner O, Pakzad H. The Evaluation of Patellar Height: A Simple Method. J Bone Joint Surg Am 2011;93:73-80. [Crossref] [PubMed]
- Biedert RM, Albrecht S. The patellotrochlear index: a new index for assessing patellar height. Knee Surg Sports Traumatol Arthrosc 2006;14:707-12. [Crossref] [PubMed]
- Andrish J. Surgical Options for Patellar Stabilization in the Skeletally Immature Patient. Sports Med Arthrosc 2007;15:82-8. [Crossref] [PubMed]
- Liu JN, Brady JM, Kalbian IL, et al. Clinical Outcomes After Isolated Medial Patellofemoral Ligament Reconstruction for Patellar Instability Among Patients With Trochlear Dysplasia. Am J Sports Med 2018;46:883-9. [Crossref] [PubMed]
Cite this article as: Andrish J. Patella instability in the skeletally immature patient: pearls for surgical treatment. Ann Joint 2018;3:38.


