
inteCartilage repair in the hip
Introduction
Chondral lesions in the hip can be the result of various etiologies, including femoroacetabular impingement (FAI), labral tear, osteochondritis dissecans, Legg-Calve-Perthes, dysplasia, traumatic subluxation or dislocation, femoral head fracture, or slipped capital femoral epiphysis. When associated with FAI, a Cam lesion at the anterolateral head-neck junction typically causes acetabular delamination, but fibrillation or focal defects can also be found (1). Unfortunately, treatment of the underlying pathology does not reliably improve the cartilage defect (2) and untreated chondral defects are known to progress to degenerative arthritis (3).
There are several options available for joint-preserving surgical treatment of chondral lesions in the hip (Table 1). The majority of these techniques have been derived from existing options for the knee (4). Surgical treatment of chondral lesions in the hip, unlike the knee, almost always includes procedures to correct the underlying pathology. Although clinically indicated, when patients undergo multiple concomitant procedures along with surgical treatment of a chondral defect, the post-operative outcome scores become difficult to interpret. Furthermore, the literature available for the hip is predominantly lower level evidence than that for the knee.
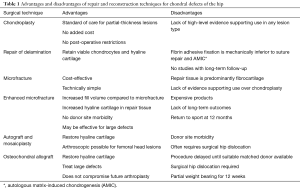
Full table
This review aims to provide an overview of the most recent available evidence for the various techniques of chondral repair and reconstruction in the hip.
Chondroplasty
Debridement of unstable partial-thickness chondral lesions has been the accepted standard of care for several years (5). However, a recent randomized controlled trial did not support debridement of these lesions in the knee. For patients undergoing arthroscopy for partial meniscectomy, Bisson et al. found no difference in outcome scores comparing debridement to observation of unstable partial- or full-thickness chondral lesions (6).
Unfortunately, there is no equally high-level evidence for the hip. Existing studies do not establish a control group and include multiple procedures, which complicates interpretation of the results. A retrospective review by Haviv et al. of 166 patients with acetabular chondral lesions associated with a Cam lesion and/or small labral tear treated partial-thickness defects with debridement and full-thickness defects less than 300 mm2 with either debridement or microfracture, depending on when the procedure was done. All patients showed significant improvements in post-operative outcome scores at last follow-up (mean 22 months). The highest scores were found in patients with partial-thickness defects, who were also younger and had higher pre-operative scores. There was no reported difference between debridement versus microfracture for full-thickness lesions (7).
In a similar prospective study of chondral lesions in FAI by Philippon et al., Outerbridge grade two and three lesions were debrided and grade four lesions were treated with microfracture. Patients also underwent femoral and/or acetabular osteoplasty and labral repair or debridement as indicated. At a mean follow-up of 2 years, all patients showed significant improvement in outcome scores with no difference between the debridement and microfracture groups (8).
Repair of delamination
Cartilage damage associated with Cam-type FAI is most commonly a delamination at the chondrolabral junction. Histological analysis of the delaminated cartilage has shown the flap retains a large proportion of viable chondrocytes and 50% of the samples contained predominantly hyaline cartilage (9). Therefore, if a stable repair of the flap could be achieved, this repaired cartilage would theoretically be of higher quality than fibrocartilage fill.
There are two described techniques for repair of delaminated cartilage, one with fibrin glue by Bray et al. (10) (Figure 1) and the other with suture anchor fixation by Sekiya et al. (11). Fibrin glue has the added benefit of promoting chondrocyte migration and proliferation (12), whereas suture anchor fixation has superior biomechanical properties, but can have issues with suture cut through (13).
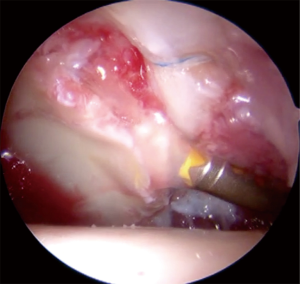
Two case series report the results of reattachment of delaminated chondral flaps using microfracture and fibrin adhesive. Stafford et al. followed 43 patients for a mean of 28 months and found a significant improvement in Modified Harris Hip Score (MHHS) (14). Tzaveas et al. reported significant improvements in MHHS at 6 and 12 months post-operatively in their series of 19 patients (15). Both studies described intact cartilage repair when patients underwent revision arthroscopy for other pathologies.
Clinical evidence for suture fixation is limited to a single case study by Sekiya et al. using polydioxanone monofilament to repair a 1-cm delaminated flap. The patient also underwent femoral osteoplasty, labral repair, iliopsoas lengthening, and capsular plication for other associated pathologies. Harris Hip Score at 2 years was 96 and there were no complications (11).
Microfracture
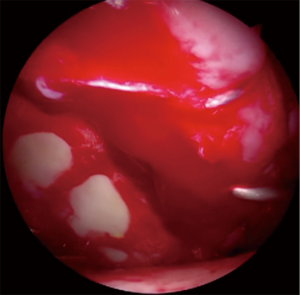
Microfracture is thought to release mesenchymal stem cells and blood from the subchondral bone to create a clot and subsequently fibrocartilage fill of the defect (Figure 2). A recent systematic review by MacDonald et al. identified mostly level IV evidence supporting the use of microfracture in chondral defects associated with FAI. Out of the 12 included studies, 11 reported positive outcomes with significant improvement in various outcome measures. However, eight of these studies did not record the size of the lesion and six did not specify the lesion location (16). Furthermore, the subsequent five-year follow-up of one of the included studies, which was described as having positive results at a mean of 36 months, showed the outcome scores in microfracture patients declined from 2 to 5 years post-operatively (17).
Even in knee literature, there is only one level I study that compares microfracture to a control (debridement) technique and found no significant difference in outcome scores between these two groups (18).
Evidence supporting microfracture for hip chondral lesions is limited to case series and studies comparing patients treated with microfracture for full-thickness lesions to patients without full-thickness defects. A matched case control of 84 microfracture patients by Domb et al. found a higher pain score and lower patient satisfaction at 2 years, compared to a matched cohort without a full-thickness chondral lesion (19). A similar comparative study by McDonald et al. in professional athletes found no difference in return to play between the cohort with a grade IV chondral lesion treated with microfracture and the control cohort with no grade IV defect (20).
Enhanced microfracture
In an attempt to improve the mechanical stability and increase hyaline cartilage content of microfracture repair tissue, several biological scaffolds have been developed. BST-CarGel (Piramal Life Sciences, Quebec, Canada) is a chitosan-based scaffold that is mixed with autologous blood and used to fill the defect in a one-step procedure (21) (Figure 3). A randomized control trial of 60 patients comparing microfracture alone to microfracture with BST-CarGel for focal full-thickness femoral condyle lesions, showed increased fill and higher quality repair cartilage in the BST-CarGel group at 1 and 5 years post-operatively (22).
The use of BST-CarGel in hip arthroscopy was recently described by Tey et al. (23). Tahoun et al. reported a series of 13 patients underwent femoroplasty, labral repair, and microfracture with BST-CarGel for a mean chondral defect of 3.7 cm2 and showed significant improvement in outcome scores at 2 years. At 18–24 months after the procedure, delayed gadolinium-enhanced MRI of cartilage for 10 patients showed greater than 90% filling of the defect in all patients and 50% had some hyaline cartilage (24). A retrospective review of 37 patients with mean chondral defect 5.8 cm2 treated with BST-CarGel showed significant improvement in outcome scores at one year post-operatively. This was regardless of defect size (2–4, 4–6, or >6 cm2), primary or revision surgery, and with or without labral reconstruction. Two patient developed significant postoperative pain, which was found to be an inflammatory response presumably from BST-CarGel (Wong I, 2017, unpublished data).
Chondro-Gide (Geistlich Pharma AG, Wolhusen, Switzerland) is a bilayer matrix of collagen type I and III that is attached to the microfractured defect with fibrin adhesive or sutures (21). For chondral defects in the knee, a randomized control trial compared microfracture alone to microfracture with Chondro-Gide secured with either sutures or fibrin glue. Outcome scores at 5 years remained stable in the Chondro-Gide groups, but significantly decreased in the microfracture group. At 2 and 5 years post-operatively, 60% of Chondro-Gide patients had greater than two-thirds defect fill on MRI, compared to 25% of microfracture patients (25).
Microfracture with Chondro-Gide was compared to two-stage matrix-associated autologous chondrocyte implantation (MACI) by Mancini and Fontana in a retrospective study of 57 patients with 2–4 cm2 acetabular chondral lesions associated with FAI. Results showed no difference in outcome scores between the techniques at 6 months, 3 years, and 5 years, but noted the benefits of Chondro-Gide as a single stage procedure with no donor site morbidity (26).
Autograft and mosaicplasty
Osteochondral autograft can be used to treat chondral lesions with associated subchondral damage and has the advantage of filling the defect with hyaline cartilage. There is the possibility of donor site morbidity and need for surgical hip dislocation, but techniques have been described for arthroscopic-assisted approaches for femoral head defects (27,28). A case report by Kocadal et al. describes a 27-year-old patient with a focal defect on the femoral head who underwent arthroscopic-assisted retrograde insertion of an osteochondral cylindrical plug harvested from the ipsilateral knee. Final follow-up of 26 months showed preservation of radiographic joint space and HHS of 96 (27). A similar technique was described by Uchida et al. for an 18-year-old patient with osteochondritis dissecans of the femoral head treated with retrograde osteochondral autograft. He also had excellent results with a MHHS of 100 at 14 months post-operatively (28).
For mosaicplasty of larger femoral defects, autograft can be harvested from the inferior non-weight bearing femoral head through a surgical hip dislocation. Girard et al. reported on a series of 10 patients who underwent mosaicplasty for a mean femoral head defect of 4.8 cm2. At the mean follow-up of 29 months, all patients had increased outcome scores, increased hip range of motion, and excellent radiographic incorporation of the osteochondral plugs (29).
Osteochondral allograft transplantation
Allograft is an acceptable option for a large chondral defect in a young patient or a chondral defect with associated subchondral injury. Allograft reconstruction of osteochondral defects of the distal femur or tibial plateau have a graft survival rate of 85% and 80%, respectively, at 10 years (30). Allograft fills the defect with hyaline cartilage and, in contrast to an osteotomy, does not complicate future arthroplasty.
A series of 17 patients, with various pathologies, underwent reconstruction of the femoral head with fresh-stored osteochondral allograft. The authors, Khanna et al., describe their indications as a contained defect greater than 2.5 cm2, involving less than 50% of the femoral head, with no significant osteoarthritis, in a patient less than 50 years old. Final HHS at a mean follow-up of 41 months was fair to good in 76%. Patients with poor outcomes had either Legg-Calve-Perthes with residual deformity and early degenerative changes or avascular necrosis (AVN) secondary to long-term steroids. Two patients with AVN induced by short-term steroids had good results (31).
Frozen osteochondral allograft has been used in a trauma case for reconstruction of the femoral head by Nousiainen et al. An 18-year-old patient with a non-repairable middle third femoral head fragment underwent acute reconstruction stabilized with countersunk bioabsorbable screws. At 46 months after surgery, he had a HHS of 100, no AVN, no pain, but some evidence of progressive arthrosis on MRI (32).
Disadvantages of this allograft reconstruction include the need of a matched donor causing a long wait time, as well as the need for a surgical hip dislocation and therefore prolonged protected weight bearing post-operatively and risk of trochanteric non-union or screw irritation.
Conclusions
The surgical treatment of chondral defects in the hip is still an evolving field. As techniques in hip arthroscopy improve, many procedures previously only used in the knee are now being applied to the hip. In the short-term, many of these options have excellent results in treating the chondral defect. Whether or not this will translate to the prevention of degenerative arthritis is yet to be determined. Although there is a lack of high-level evidence for treatment of chondral lesions in the hip, there are clear advantages and disadvantages to the different surgical techniques that can help guide decision-making for individual patients.
Acknowledgments
Funding: None.
Footnote
Provenance and Peer Review: This article was commissioned by the Guest Editors (Olufemi R. Ayeni and Ryan P. Coughlin) for the series “Future Perspectives in Hip Preservation and Arthroscopy” published in Annals of Joint. The article has undergone external peer review.
Conflicts of Interest: Both authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/aoj.2018.03.08). The series “Future Perspectives in Hip Preservation and Arthroscopy” was commissioned by the editorial office without any funding or sponsorship. The authors have no other conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Ellis HB, Briggs KK, Philippon MJ. Innovation in hip arthroscopy: is hip arthritis preventable in the athlete? Br J Sports Med 2011;45:253-8. [Crossref] [PubMed]
- Suzuki C, Harada Y, Mitsuhashi S. Repair of cartilage defects and torn acetabular labrum in hip joints after conventional osteotomy: evaluation by follow-up arthroscopy. J Orthop Sci 2005;10:127-32. [Crossref] [PubMed]
- Beck M, Kalhor M, Leunig M, Ganz R. Hip morphology influences the pattern of damage to the acetabular cartilage: femoroacetabular impingement as a cause of early osteoarthritis of the hip. J Bone Joint Surg Br 2005;87:1012-8. [Crossref] [PubMed]
- Bedi A, Feeley BT, Williams RJ. Management of articular cartilage defects of the knee. J Bone Joint Surg Am 2010;92:994-1009. [Crossref] [PubMed]
- Montgomery SR, Foster BD, Ngo SS, et al. Trends in the surgical treatment of articular cartilage defects of the knee in the United States. Knee Surg Sports Traumatol Arthrosc 2014;22:2070-5. [Crossref] [PubMed]
- Bisson LJ, Kluczynski MA, Wind WM, et al. Patient outcomes after observation versus debridement of unstable chondral lesions during partial meniscectomy. J Bone Joint Surg Am 2017;99:1078-85. [Crossref] [PubMed]
- Haviv B, Singh PJ, Takla A, et al. Arthroscopic femoral osteochondroplasty for cam lesions with isolated acetabular chondral damage. J Bone Joint Surg Br 2010;92:629-33. [Crossref] [PubMed]
- Philippon MJ, Briggs KK, Yen YM, et al. Outcomes following hip arthroscopy for femoroacetabular impingement with associated chondrolabral dysfunction: minimum two-year follow-up. J Bone Joint Surg Br 2009;91:16-23. [Crossref] [PubMed]
- Meulenkamp B, Gravel D, Beaulé PE. Viability assessment of the chondral flap in patients with cam-type femoroacetabular impingement: a preliminary report. Can J Surg 2014;57:44-8. [Crossref] [PubMed]
- Bray ED, Barke SJ, Stafford GH, et al. Surgical technique: Microfracture and fibrin glue for cartilage delamination. In: Nho SH, Leunig M, Larson CM, et al. editors. Hip Arthroscopy and Hip Joint Preservation Surgery. New York: Springer, 2015:1107-15.
- Sekiya JK, Martin RL, Lesniak BP. Arthroscopic repair of delaminated acetabular articular cartilage in femoroacetabular impingement. Orthopedics 2009;32:692-6. [Crossref] [PubMed]
- Kirilak Y, Pavlos NJ, Willers CR, et al. Fibrin sealant promotes migration and proliferation of human articular chondrocytes: possible involvement of thrombin and protease-activated receptors. Int J Mol Med 2006;17:551-8. [PubMed]
- Cassar-Gheiti AJ, Byrne DP, Kavanagh E, et al. Comparison of four chondral repair techniques in the hip joint: A biomechanical study using a physiological human cadaveric model. Osteoarthritis Cartilage 2015;23:1018-25. [Crossref] [PubMed]
- Stafford GH, Bunn JR, Villar RN. Arthroscopic repair of delaminated acetabular articular cartilage using fibrin adhesive. Results at one to three years. Hip Int 2011;21:744-50. [Crossref] [PubMed]
- Tzaveas AP, Villar RN. Arthroscopic repair of acetabular chondral delamination with fibrin adhesive. Hip Int 2010;20:115-9. [Crossref] [PubMed]
- MacDonald AE, Bedi A, Horner NS, et al. Indications and outcomes for microfracture as an adjunct to hip arthroscopy for treatment of chondral defects in patients with femoroacetabular impingement: A systematic review. Arthroscopy 2016;32:190-200.e2. [Crossref] [PubMed]
- Fontana A, de Girolamo L. Sustained five-year benefit of autologous matrix-induced chondrogenesis for femoral acetabular impingement-induced chondral lesions compared with microfracture treatment. Bone Joint J 2015;97-B:628-35. [Crossref] [PubMed]
- Gudas R, Gudaite A, Mickevicius T, et al. Comparison of osteochondral autologous transplantation, microfracture, or debridement techniques in articular cartilage lesions associated with anterior cruciate ligament injury: A prospective study with a 3-year follow-up. Arthroscopy 2013;29:89-97. [Crossref] [PubMed]
- Domb BG, Gupta A, Dunne KF, et al. Microfracture in the hip: Results of a matched-cohort controlled study with 2-year follow-up. Am J Sports Med 2015;43:1865-74. [Crossref] [PubMed]
- McDonald JE, Herzog MM, Philippon MJ. Return to play after hip arthroscopy with microfracture in elite athletes. Arthroscopy 2013;29:330-5. [Crossref] [PubMed]
- Jeuken RM, Roth AK, Peters RW, et al. Polymers in cartilage defect repair of the knee: Current status and future prospects. Polymers 2016;8:219. [Crossref]
- Shive MS, Stanish WD, McCormack R, et al. BST-CarGel® treatment maintains cartilage repair superiority over microfracture at 5 years in a multicenter randomized controlled trial. Cartilage 2015;6:62-72. [Crossref] [PubMed]
- Tey M, Mas J, Pelfort X, et al. Arthroscopic treatment of hip chondral defect with bone marrow stimulation and BST-CarGel. Arthrosc Tech 2015;4:e29-e33. [Crossref] [PubMed]
- Tahoun M, Shehata TA, Ormazabal I, et al. Results of arthroscopic treatment of chondral delamination in femoroacetabular impingement with bone marrow stimulation and BST-CarGel®. SICOT J 2017;3:51. [Crossref] [PubMed]
- Volz M, Schaumburger J, Frick H, et al. A randomized controlled trial demonstrating sustained benefit of Autologous Matrix-Induced Chondrogenesis over microfracture at five years. Int Orthop 2017;41:797-804. [Crossref] [PubMed]
- Mancini D, Fontana A. Five-year results of arthroscopic techniques for the treatment of acetabular chondral lesions in femoroacetabular impingement. Int Orthop 2014;38:2057e64.
- Kocadal O, Akman B, Guven M, et al. Arthroscopic-assisted retrograde mosaicplasty for an osteochondral defect of the femoral head without performing surgical hip dislocation. SICOT J 2017;3:41. [Crossref] [PubMed]
- Uchida S, Utsunomiya H, Honda E, et al. Arthroscopic osteochondral autologous transplantation for the treatment of osteochondritis dissecans of the femoral head. SICOT J 2017;3: [Crossref]
- Girard J, Roumazeille T, Sakr M, et al. Osteochondral mosaicplasty of the femoral head. Hip Int 2011;21:542-8. [Crossref] [PubMed]
- Gross AE, Shasha N, Aubin P. Long-term follow up of the use of fresh osteochondral allografts for posttraumatic knee defects. Clin Orthop Relat Res 2005;79-87. [Crossref] [PubMed]
- Khanna V, Tushinski DM, Drexler M, et al. Cartilage restoration of the hip using fresh osteochondral allograft. Bone Joint J 2014;96:11-16. [Crossref] [PubMed]
- Nousiainen MT, Sen MK, Mintz DN, et al. The use of osteochondral allograft in the treatment of a severe femoral head fracture. J Orthop Trauma 2010;24:120-4. [Crossref] [PubMed]
Cite this article as: Gordey EE, Wong IH. inteCartilage repair in the hip. Ann Joint 2018;3:24.



