Don’t forget the open Bankart—Look at the evidence
Introduction
The glenohumeral joint is the most frequently dislocated joint in the body, because of its inherently unstable bony morphology (1). The glenoid labrum is one of the structures that improves shoulder stability, by deepening the shallow glenoid fossa to improve its articulation with the humeral head. Bankart lesions, a detachment of the joint capsule and labrum from the anterior glenoid rim with or without a bone fragment, have been identified in as many as 85% of shoulder dislocations (2,3). Historically, the gold-standard solution for the surgical treatment of anterior shoulder instability has been an open Bankart repair (3-11). This approach allows surgeons to directly visualize the glenohumeral joint, accomplish a large capsular shift and guarantee a complete repair of the anteroinferior capsulolabral tissue (12).
As arthroscopic procedure techniques have greatly evolved and improved over the last decade, a shift occurred that favors the arthroscopic approach (5,7,10,11,13,14). The advantages of arthroscopy include shorter operative time, a smaller incision, preservation of the subscapularis tendon, decreased morbidity, the ability to concurrently address other associated intra-articular pathology, including the posterior labrum, and faster recovery of range of motion (4,5,8-10,12). Initially the failure rates were high; however, the use of at least 3 suture anchors are thought to provide a superior result (3,6-9,14). A recent systematic review suggests that by excluding patient with significant bone loss, using 3 or more anchors, and performing the surgery in the lateral decubitus position, the recurrence rate decreases from 17.8% to 7.9% for collision athletes (15).
Despite progressive use of modern arthroscopic Bankart repair techniques, there are concerning findings that this approach offers inferior outcomes regarding recurrent instability, recurrent dislocation/subluxation, reoperation rates, and persistent capsular laxity (3,6,12,16,17). Patients that participate in contact sports, have physically demanding activities or work, aged less than 25 years, or suffering from bone loss or hyperlaxity experience additional risk (3,14,18). We will examine the evidence for the use of the open Bankart today, describe our surgical technique and offer clinical pearls in this chapter.
Review of the literature
Open Bankart long term outcomes
One of the most important criteria for determining success with any surgical procedure is the maintenance of good outcomes with long-term follow-up. Studies examining the open Bankart procedure have in general longer follow ups than arthroscopic Bankart, with more historical precedence. In 1978, Rowe reported the failure rates after open shoulder stabilization for recurrent anterior instability to range between 3% to 9% (19). In a 25-year follow up study, Fabre et al. reported excellent patient-reported outcomes for the open Bankart procedure with no statistically significant loss of motion and a 16% recurrence rate (20). Like many long-term shoulder instability outcome studies, the authors found 69% of patients showed radiographic signs of osteoarthritis at latest follow-up. Berendes et al. found a lower recurrent instability rate of 9.7% over 10 years using a modified open Bankart procedure with suture anchors (21). In the absence of substantial osseous glenoid defect, Moroder et al. found a recurrence rate of 17.5% and revision rate of 4.2% at a minimum of 20 years in a study of 47 patients, most without symptoms for at least eight years postoperatively (22); Arthroscopic Bankart using suture anchors has reported recurrence rates of up to 10% after 3.6 years, 14–38% after 5 years, and 23–35% after 10.9 years (8,14,21).
Results in contact athletes
Collision athletes have been found to be at an increased risk for redislocation following Bankart procedures due to the high physical demand of the activity, yielding 11–16.5% postoperative subluxation or dislocation after an average of 3 years (18). Rhee et al. found that in this patient population, arthroscopy resulted in a higher failure rate than open Bankart repair (18). The authors found a 25% recurrent instability rate following arthroscopic surgery and 12.5% recurrence rate following open Bankart repair. Similarly, Yamamoto et al. found contact athletes had two times higher recurrence rate in the open group and three times higher in the arthroscopic group compared to that of non-contact athletes (23). In a study of 103 patients (majority were collision athletes) treated with open Bankart repair, Pagnani only found two recurrences (24). Interestingly, the author found that bone loss of the humeral head or glenoid did not appear to result in a significant increase in the risk of recurrence with conventional open techniques of stabilization, as has been shown with arthroscopic techniques. These results show that open Bankart may be a better choice than arthroscopic Bankart in the contact athlete population; however, these contact athletes remain a difficult population to treat with higher recurrence rates than normal.
Results in the revision setting
Revision of failed arthroscopic Bankart repair is also another area where open Bankart may be useful. De Giorgi et al. reported a 36% failure rate when arthroscopic Bankart was used again in the revision setting (25). In contrast, Cho et al. found a lower recurrence rate of 11.5%, when revising initial arthroscopic Bankart with an open Bankart repair (10). In a ten year follow up study, Neviaser used the open Bankart procedure to revise thirty prior failed stabilizations (26). Twenty-two of the twenty-three athletes returned to play. No recurrences or revisions were found. The authors concluded that the open Bankart repair offers a reliable, consistently successful option for revision of failed stabilizations.
Direct comparison studies between arthroscopic and open Bankart
There’s a lack of high quality randomized level one studies comparing open versus arthroscopic Bankart techniques. Sperber conducted a randomized study in 56 patients with minimum two year follow up. They found the recurrent instability rate to be 23% in the arthroscopic group and 12% in the open group, however this did not reach statistical significance (27). Fabbriciani’s prospective study involved 60 patients evenly divided into two groups. They reported no recurrences in either group and similar constant scores (28). Bottoni conducted a randomized study in 61 patients; twenty-nine with open technique and thirty with arthroscopic techniques. Both techniques yielded similar subjective and objective outcomes, and similar recurrence rates (29). However, the above studies may have been underpowered given the small sample sizes to detect a difference in recurrence rates. Mohtadi et al. conducted a similar randomized study in 2014 with over 180 patients and powered appropriately to look for recurrence (30). In this study, Mohtadi found that recurrence rates at two years were significantly lower in the open group at 11% compared to the arthroscopic group at 23% (30). Similar WOSI and ASES scores were observed in both groups. Along the same lines, in a retrospective comparison, Guanche et al. found open Bankart had 0% recurrence rate compared to 33% in arthroscopic Bankart (31). They concluded that open Bankart leads to better satisfaction, stability, range of motion, and a lower recurrence of subluxation/dislocation (31). Virk et al. found no statistical difference in failure rates, but did find arthroscopy to have a significantly shorter time to recurrence of instability (9). Freedman et al. reported arthroscopic Bankart to have a significantly higher rate of recurrent dislocation at 20.3% than open Bankart repair at 10.3%. In addition, the authors reported a higher proportion of patients with an excellent or good postoperative Rowe score in the open group (88%) than in the arthroscopic group (71%) (32). A meta-analysis by Mohtadi et al. showed that an open repair for recurrent traumatic anterior instability has a lower recurrent and faster return to activity (11). In addition, there’s also level one evidence that there are no side-to-side isokinetic strength deficits between patients having an open stabilization using a subscapularis splitting approach versus arthroscopic stabilization (33).
Surgical technique
Exam under anesthesia should always be conducted first to check for engagement of the Hill Sachs lesion, grading of the load-shift, posterior and multi-directional instability, and comparison to the contralateral shoulder. After examination under anesthesia, the patient was positioned in a modified beach-chair position with a small bump underneath the scapula to protract the scapula forward.
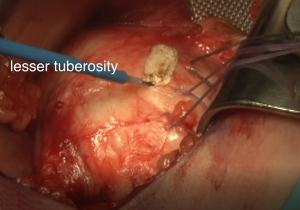
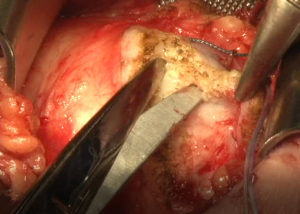
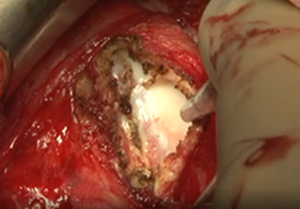
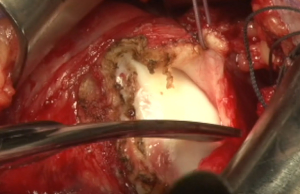
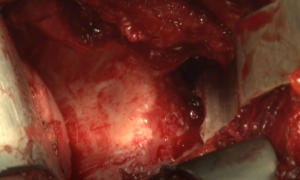
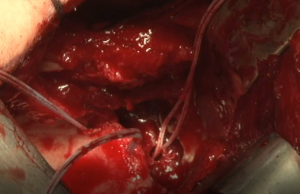
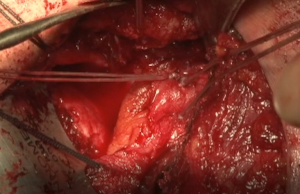
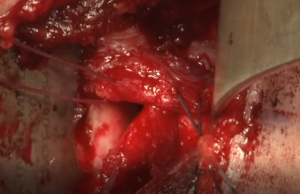
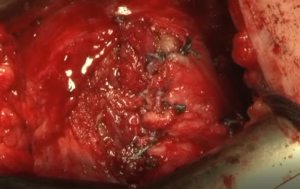
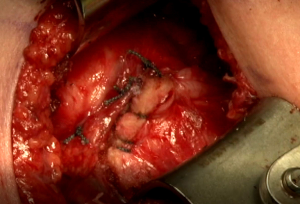
The open stabilization technique consisted of an anterior axillary incision, following the deltopectoral interval retracting the cephalic vein laterally. Next, the clavipectoral fascia is incised and the conjoined tendon is retracted medially and the subscapularis tendon exposed. If the patient has significant capsular laxity, we prefer to perform a subscapularis tenotomy because it allows us to perform a more extensive capsular shift. We tenotomized the subscapularis tendon longitudinally 1.5cm from its insertion on the lesser tuberosity (Figure 1); the tendon is tagged and carefully separated from the underlying capsule (Figure 2). The rotator interval lesion along with any capsular defects superiorly is first closed in a side-to-side manner with absorbable suture. It is important to only close the lateral most aspect of the interval with the arm in external rotation to not restrict motion. A longitudinal capsular incision along the anatomic neck insertion was followed by a horizontal capsulotomy to the anteroinferior labrum to create inferior and superior capsule leaflets to allow for exposure and subsequent capsular shift (Figures 3,4).
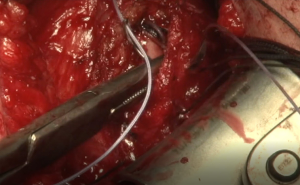
A humeral head retractor such as a Fukuda is then placed laterally and a retractor placed medially along the scapular neck to expose the Bankart lesion (Figure 5). A burr is used to decorticate the neck to facilitate bony healing. Anatomical labral repair is performed with double loaded suture anchors from inferior to superior along the anterior rim at the 6, 5, 4 and 3 o’clock position. In bigger lesions, a double row repair can be made with anchors placed more medially along the scapular neck (Figure 6). Sutures from the anchors are passed in a mattress configuration and tied (Figure 7).
A lateral-based capsular shift is then used to eliminate redundancy in the axillary pouch. The inferior leaflet of the capsule is shifted superiorly and laterally, and attached to the humeral neck with suture anchors (Figure 8); the superior leaflet is shifted and attached inferiorly and laterally, overlapping the inferior leaflet. We use a “pants over vest” suture medially by advancing the inferior leaflet superiorly and then reinforcing the repair with the overlapping superior leaflet (Figure 9). The shoulder should be completely stable at this point with the completion of the capsular repair (Figure 10).
Anatomical repair of the subscapularis tendon is performed with high tensile nonabsorbable suture (Figure 11). The soft tissue and skin is closed in layers and patient immobilized in a sling for four weeks.
Clinical pearls
- The separation between subscapularis tendon and the underlying capsule is done easier if started inferiorly, where there is a more defined tissue interval. This is typically just superior to the anterior circumflex vessels.
- We prefer to use self-retaining retractors such as a Cobell for retraction. However, these can slip over the course of the case, and constant attention should be paid to place the medial paddle as inferior as possible for better visualization of the anterior inferior glenoid.
- We routinely close the rotator interval particularly in lax patients with a sulcus sign. We like to do this laterally, and not medially.
- A subscapularis split approach can also be used if just a labral repair needs to be made, such as in the setting of a bony Bankart lesion. However, we prefer to perform a subscapularis tenotomy because it allows us to perform a more extensive capsular shift.
- For a subscapularis split approach, the muscle is split in a horizontal fashion at the interval between the upper 2/3rd and lower 1/3 of the muscle. The muscle is reflected off the capsule and then a horizontal capsulotomy is made. The Bankart lesion can be performed and a capsular shift can be performed, shifting the inferior capsule superiorly to eliminate antero-inferior redundancy.
- The repair of the subscapularis can be done also with sutures from the anchors placed for capsular shift for added security.
Acknowledgments
Funding: None.
Footnote
Provenance and Peer Review: This article was commissioned by the Guest Editors (Albert Lin and Jason J. Shin) for the series “Trends in Anterior Shoulder Instability” published in Annals of Joint. The article has undergone external peer review.
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/aoj.2017.10.10). The series “Trends in Anterior Shoulder Instability” was commissioned by the editorial office without any funding or sponsorship. The authors have no other conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Sedeek SM, Bin Abd Razak HR, Ee GWW, et al. First-time anterior shoulder dislocations: should they be arthroscopically stabilised? Singapore medical journal 2014;55:511-5; quiz 516 [Crossref] [PubMed]
- Widjaja AB, Tran A, Bailey M, et al. Correlation Between Bankart and Hill-Sachs Lesions in Anterior Shoulder Dislocation. ANZ Journal of Surgery 2006;76:436-8. [Crossref] [PubMed]
- Boileau P, Villalba M, Héry J-Y, et al. Risk Factors for Recurrence of Shoulder Instability After Arthroscopic Bankart Repair. The Journal of Bone & Joint Surgery 2006;88:1755-63. [PubMed]
- Coughlin RP, Crapser A, Coughlin K, et al. Open Bankart Revisited. Arthroscopy Techniques 2017;6:e233-7. [Crossref] [PubMed]
- Zhang AL, Montgomery SR, Ngo SS, et al. Arthroscopic versus open shoulder stabilization: current practice patterns in the United States. Arthroscopy: the journal of arthroscopic & related surgery 2014;30:436-43. [Crossref] [PubMed]
- Kim S-H, Ha K-I, Cho Y-B, et al. Arthroscopic Anterior Stabilization of the Shoulder Two to Six-Year Follow-up. The Journal of Bone & Joint Surgery 2003;85-A:1511-8. [Crossref] [PubMed]
- Castagna A, Markopoulos N, Conti M, et al. Arthroscopic bankart suture-anchor repair: radiological and clinical outcome at minimum 10 years of follow-up. Am J Sports Med 2010;38:2012-6. [Crossref] [PubMed]
- van der Linde JA, van Kampen DA, Terwee CB, et al. Long-term results after arthroscopic shoulder stabilization using suture anchors: an 8- to 10-year follow-up. Am J Sports Med 2011;39:2396-403. [Crossref] [PubMed]
- Virk MS, Manzo RL, Cote M, et al. Comparison of Time to Recurrence of Instability After Open and Arthroscopic Bankart Repair Techniques. Orthopaedic Journal of Sports Medicine 2016;4:2325967116654114 [Crossref] [PubMed]
- Cho NS, Yi JW, Lee BG, et al. Revision open Bankart surgery after arthroscopic repair for traumatic anterior shoulder instability. The American Journal of Sports Medicine 2009;37:2158-64. [Crossref] [PubMed]
- Mohtadi NGH, Bitar IJ, Sasyniuk TM, et al. Arthroscopic Versus Open Repair for Traumatic Anterior Shoulder Instability: A Meta-analysis. Arthroscopy: The Journal of Arthroscopic and Related Surgery 2005;21:652-8. [Crossref] [PubMed]
- Chen L, Xu Z, Peng J, et al. Effectiveness and safety of arthroscopic versus open Bankart repair for recurrent anterior shoulder dislocation: a meta-analysis of clinical trial data. Archives of orthopaedic and trauma surgery 2015;135:529-38. [Crossref] [PubMed]
- Owens BD, Harrast JJ, Hurwitz SR, et al. Surgical Trends in Bankart Repair: An Analysis of Data From the American Board of Orthopaedic Surgery Certification Examination. The American Journal of Sports Medicine 2011;39:1865-9. [Crossref] [PubMed]
- Voos JE, Livermore RW, Feeley BT, et al. Prospective evaluation of arthroscopic bankart repairs for anterior instability. Am J Sports Med 2010;38:302-7. [Crossref] [PubMed]
- Leroux TS, Saltzman BM, Meyer M, et al. The Influence of Evidence-Based Surgical Indications and Techniques on Failure Rates After Arthroscopic Shoulder Stabilization in the Contact or Collision Athlete With Anterior Shoulder Instability. Am J Sports Med 2017;45:1218-25. [Crossref] [PubMed]
- Lenters TR. Arthroscopic Compared with Open Repairs for Recurrent Anterior Shoulder Instability A Systematic Review and Meta-Analysis of the Literature. J Bone Joint Surg Am 2007;89:244-54. [PubMed]
- Park J-Y, Chung SW, Kumar G, et al. Factors Affecting Capsular Volume Changes and Association With Outcomes After Bankart Repair and Capsular Shift. The American Journal of Sports Medicine 2015;43:428-38. [Crossref] [PubMed]
- Rhee YG, Ha JH, Cho NS. Anterior shoulder stabilization in collision athletes: arthroscopic versus open Bankart repair. The American journal of sports medicine 2006;34:979-85. [Crossref] [PubMed]
- Rowe CR, Patel D, Southmayd WW. The Bankart procedure: a long-term end-result study. The Journal of bone and joint surgery American volume 1978;60:1. [Crossref] [PubMed]
- Fabre T, Abi-Chahla ML, Billaud A, et al. Long-term results with Bankart procedure: A 26-year follow-up study of 50 cases. Journal of Shoulder and Elbow Surgery 2010;19:318-23. [Crossref] [PubMed]
- Berendes TD, Wolterbeek R, Pilot P, et al. The open modified Bankart procedure: outcome at follow-up of 10 to 15 years. The Journal of bone and joint surgery British volume 2007;89:1064-8. [Crossref] [PubMed]
- Moroder P, Odorizzi M, Pizzinini S, et al. Open Bankart Repair for the Treatment of Anterior Shoulder Instability without Substantial Osseous Glenoid Defects: Results After a Minimum Follow-up of Twenty Years. The Journal of bone and joint surgery American volume 2015;97:1398-405. [Crossref] [PubMed]
- Yamamoto N, Kijima H, Nagamoto H, et al. Outcome of Bankart repair in contact versus non-contact athletes. Orthopaedics & traumatology, surgery & research OTSR 2015;101:415-9. [PubMed]
- Pagnani MJ. Open capsular repair without bone block for recurrent anterior shoulder instability in patients with and without bony defects of the glenoid and/or humeral head. Am J Sports Med 2008;36:1805-12. [Crossref] [PubMed]
- De Giorgi S, Garofalo R, Tafuri S, et al. Can arthroscopic revision surgery for shoulder instability be a fair option? Muscles, ligaments and tendons journal 2014;4:226-31. [PubMed]
- Neviaser AS, Benke MT, Neviaser RJ. Open Bankart repair for revision of failed prior stabilization: outcome analysis at a mean of more than 10 years. J Shoulder Elbow Surg 2015;24:897-901. [Crossref] [PubMed]
- Sperber A, Hamberg P, Karlsson J, et al. Comparison of an arthroscopic and an open procedure for posttraumatic instability of the shoulder: a prospective, randomized multicenter study. J Shoulder Elbow Surg 2001;10:105-8. [Crossref] [PubMed]
- Fabbriciani C, Milano G, Demontis A, et al. Arthroscopic versus open treatment of Bankart lesion of the shoulder: a prospective randomized study. Arthroscopy 2004;20:456-62. [Crossref] [PubMed]
- Bottoni CR, Smith EL, Berkowitz MJ, et al. Arthroscopic versus open shoulder stabilization for recurrent anterior instability: a prospective randomized clinical trial. The American journal of sports medicine 2006;34:1730-7. [Crossref] [PubMed]
- Mohtadi NGH, Chan DS, Hollinshead RM, et al. A randomized clinical trial comparing open and arthroscopic stabilization for recurrent traumatic anterior shoulder instability: two-year follow-up with disease-specific quality-of-life outcomes. The Journal of bone and joint surgery American volume 2014;96:353-60. [Crossref] [PubMed]
- Guanche CA, Quick DC, Sodergren KM, et al. Arthroscopic versus open reconstruction of the shoulder in patients with isolated Bankart lesions. The American journal of sports medicine 1996;24:144-8. [Crossref] [PubMed]
- Freedman KB, Smith AP, Romeo AA, et al. Open Bankart repair versus arthroscopic repair with transglenoid sutures or bioabsorbable tacks for Recurrent Anterior instability of the shoulder: a meta-analysis. The American journal of sports medicine 2004;32:1520-7. [Crossref] [PubMed]
- Hiemstra LA, Sasyniuk TM, Mohtadi NG, et al. Shoulder strength after open versus arthroscopic stabilization. The American Journal of Sports Medicine 2008;36:861-7. [Crossref] [PubMed]
Cite this article as: Sanborn L, Arciero RA, Yang JS. Don’t forget the open Bankart—Look at the evidence. Ann Joint 2017;2:67.