
Indications and results of high tibial osteotomy
Introduction
In varus malalignment of the lower extremity, load is abnormally transmitted across the medial tibiofemoral compartment, increasing the stress on the articular cartilage, the subchondral bone and the medial meniscus. Therefore, axial malalignment plays an important role in the development and the progression of osteoarthritis (OA) (1).
The medial opening wedge (MOW) high tibial osteotomy (HTO) was first described by Debeyre and Patte in 1951 (2). Formerly intended as a definitive treatment strategy for medial compartment knee OA, HTO became a widespread procedure in the treatment of unicompartmental OA of the knee. The leading intent of HTO is to transfer the load of the knee joint correcting the mechanical axis of the lower extremity in order to reduce pain, slow down the degenerative OA process and avoid or delay the joint replacement (3,4). Lately, due to the success of total and unicompartmental knee replacement (TKR and UKR), HTO fell out of favour, particularly for older or lower demand patients (5).
In the 1990s, the underlined role of correction of varus malalignment in sport medicine, for the treatment of ligamentous injuries and imbalance of the knee, led to a progressive reappreciation of HTO (6). Moreover, the concerns over activity restrictions, implant survival and patient satisfaction related to TKR and UKR, solicited surgeons to find any effective alternative to arthroplasty among younger and more active patients (1). In recent years, the technical advances in cartilage healing surgery and meniscal transplantation increased interest in HTO as an adjunctive procedure in order to correct axial malalignment (7).
At last, although instability was originally considered a contraindication to HTO, nowadays, a distinct indication of HTO is the correction of load imbalance in ligamentous insufficiency in order to unload or substitute any ligament reconstruction (3).
Indications
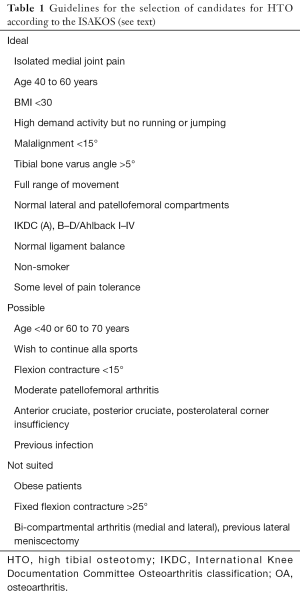
The main indication for HTO is the correction of varus malalignment in medial unicompartmental OA of the knee. In 2005, the International Society of Arthroscopy, Knee Surgery and Orthopedic Sports Medicine (ISAKOS) developed its highly accepted protocol that defined ideal patients, possible patients and patients not suited for osteotomies (8) (Table 1). Despite the time passed, these indications are still observed, with little adjustments. An ideal patient for HTO is a moderately active, high-demand, young patient (between 40–60 years old) with isolated joint line tenderness, BMI <30, malalignment <15°, metaphyseal varus (tibial bone varus angle, TBVA >5°), full range of motion (ROM), near-normal lateral and patellofemoral compartments, without ligamentous instability, non-smoker, and with some level of pain tolerance.
Full table
HTO is usually contraindicated in patients older than 65 years or with severe OA of the medial compartment (Ahlback grade III or higher), tricompartmental OA, relevant patellofemoral OA, ROM <120° (flexion less than 90° and a flexion contracture greater than 10°), joint instability and ≥1 cm lateral tibial thrust, ≥20° of malalignment (9,10); other contraindications are axial deformity correctable by physical examination and assessed on stress radiographs, diagnosed inflammatory arthritis, large area of exposed bone on tibial and femoral articular surface (>15 cm × 15 mm) and heavy smokers (11-15).
Clinical examination should assess a constitutional varus morphotype with elective tenderness at the medial joint line, asymptomatic lateral and patellofemoral compartments and should exclude abnormal ligamentous laxity, limb length discrepancy, ankle deformity and alterations of gait pattern, especially varus thrust. Patient’s previous procedures should be accurately documented, for example, a preceding meniscectomy or a ligament reconstruction.
Medial compartment narrowing is basically demonstrated by less than 4 mm of medial joint space on a standard radiographic anteroposterior image (16). For a complete preoperative radiographic assessment, multiple X-ray views are suggested: bilateral weight-bearing anteroposterior and lateral views of the lower limbs in full extension, tunnel views with the knee in 30° of flexion, Rosenberg views with the knee in 45° of flexion, lateral weight-bearing views, and skyline patellar views. Optional stress radiographs can be performed to assess ligamentous laxity and magnetic resonance imaging (MRI) can be suggested to exclude concomitant injuries as meniscal tears, ligamentous lesions, osteochondral defects, osteonecrosis or subchondral edema (9,10).
The mechanical axis is determined on the weight-bearing anteroposterior view of the lower limb in full extension, drawing a straight line from the center of the femoral head through the center of the talar dome; a varus malalignment is confirmed when the mechanical axis is situated medial to the apex of the medial tibial eminence, or more than 41% across the tibial plateau in the coronal plane with the medial border considered 0% and the lateral border 100% (17). The TBVA is determined as the angle between the axis of the proximal tibial epiphisis and the mechanical axis of the tibial bone (Figure 1). At last, the patellar height should be measured on lateral views.

The two most commonly used surgical techniques for HTO are the lateral closing wedge (LCW) and MOW HTO. The LCW technique was largely used in past years as a primary stable correction with a high rate of consolidation, but was progressively less used due to some disadvantages: bone loss with large corrections resulting in marked shortening of the leg, changes in tibial condylar offset which can complicate later TKR and surgical difficulties as the risk of peroneal nerve injuries, the need of fibular osteotomy or separation of the proximal tibiofibular joint and the need of detachment of the extensor muscles (18). Conversely, the MOW technique does not result in any bone loss but needs to be fixed with a plate, so it has progressively regained interest with the development of more stable implants which enabled the surgeon to avoid bone grafts in most cases; disadvantages are higher risks of tibial slope changes and medial collateral ligament tightening. However, a recent Cochrane review showed no evidence as to whether LCW or MOW is more effective in the treatment of symptomatic medial knee OA (19). Other HTO techniques include dome osteotomy and progressive callus distraction using an external fixator: these techniques are useful for polyaxial corrections and early weight bearing without any changes in the patellar height; however, external fixation can cause discomfort, pin tract infections and loss of correction after fixator removal. At last, a relatively new technique, the combined wedge osteotomy (CWO), merges the advantages together with some disadvantages of both techniques in a challenging procedure, and it is mainly reserved to cases which require a great deformity correction (20).
Few technical modifications of MOW HTO improved its safety and reproducibility, contributing to its growing diffusion. The introduction of the biplanar osteotomy, consisting in a second ascending coronal cut underneath the tibial tuberosity in addition to the transverse osteotomy of the posterior tibia, increases the rotational stability and creates an anterior buttress against sagittal tilting of the osteotomy. The introduction of the incomplete osteotomy, leaving intact about 10 mm of lateral bone stock with gradual opening of the gap over several minutes by sequential impaction of flat chisels or by use of a special spreading tool, permits to avoid lateral hinge fractures and increases stability too. In closing, the technical advances in plate and hardware design, produce a stable fixation and allow early mobilization and weight bearing avoiding loss of correction (18) (Figure 2).

Regarding patellar height, some authors recommend to avoid LCW HTO when the patella is already very high, as to avoid MOW HTO when the patella is lower than normal. A combined osteotomy (tibial tubercle osteotomy and HTO) permits the avoidance of patellar height change, or the correction of abnormal patellar height. Morbidity secondary to patella alta or patella baja has been investigated in several studies, often with confusing results due to the array of different methods used to measure patellar height (Insall-Salvati, Blackburne-Peel, and Caton-Deschamps) and to the presence of postoperative patellar tendon contracture as a bias. However, tibial slope changes and patellar tendon contractures can be largely avoided by assiduous attention to surgical technique for the former and early ROM exercises for the latter (21).
Regarding the materials eventually used in MOW HTO to fill the osteotomy gap, several solutions have been routinely used such as autograft, allograft, synthetic bone substitutes (hydroxyapatite, b-tricalcium phosphate, a combination of both and bone cement) with or without platelet-rich plasma, growth factors, and bone marrow concentrate. Bone graft is considered the gold standard because of its osteoconductive, osteoinductive, and osteogenic properties. Bone substitutes avoid donor site morbidity associated with bone autograft, but provide weaker resistance to compressive loading forces. Nowadays, gaps of less than 10 mm are usually left unfilled since no pseudarthrosis or loss of correction was observed in large series of patients, with ossification of the gap always progressing from the lateral hinge towards the medial side, filling at least 75% of the gap within 6−18 months (18,22).
Recently, some authors are exploring the choice of a computer-assisted navigation in HTO. Song et al. sustained that its major benefit lies in the improved accuracy and precision of postoperative coronal and sagittal alignments; in addition, the navigation system can allow a precise adjustment of the hinge axis position and reduce the risk of opposite cortical hinge fracture. However, additional studies are necessary to determine whether the improvement in alignment and hinge axis influences the long-term results and survival rates (23).
Although ligament insufficiency was originally considered a contraindication to HTO, nowadays, a second indication of HTO is the treatment of ligament deficient knees, as biomechanical studies have shown that planned alterations of the posterior tibial slope can improve or restore stability in the sagittal plane (24). Furthermore, HTO can correct load imbalance in inveterate ligament deficiency of the anterior cruciate ligament (ACL), posterolateral corner (PLC) and posterior cruciate ligament (PCL), in order to change the axial alignment, thereby reducing the varus thrust (3). In summary, the main goals for HTO in ligament deficient knees are: to prevent further medial compartment deterioration and articular cartilage wear, to protect a graft from abnormally high stress in a malaligned knee, and to restore stability (25). HTO is currently considered as a preferred alternative to a knee arthroplasty in young patients with degenerative changes and concomitant cruciate injuries, particularly in athletic active population or physically demanding workers (26). MOW HTO, in particular, allowing to alter the tibial slope easily and correcting both the coronal and sagittal plane, can produce a significant improvement in stability and function: slope should be increased in PCL deficiency and reduced in ACL deficiency (25,27). With regards to ACL deficiency and varus alignment, there is evidence to suggest that the posterior tibial slope should be decreased when it is greater than 13° in chronic ACL deficiency (28).
In the current practice, HTO can protect or substitute a ligament reconstruction in acute or chronic ACL deficient knees on the basis of patient’s age, activity level and reported instability; however, as evidenced by the literature, there is a great deal of heterogeneity in this patient population, and actually no bright algorithm exists for treatment (29). In chronic posterolateral instability, for example in cases of PCL or PLC injury, possibly associated with an ACL injury, the treatment of choice is usually an HTO alone, with a delayed PCL reconstruction in case of residual instability in a two-stage procedure (30-32).
Results
A recent systematic review reported that HTO is an effective procedure reducing pain and improving knee function in patients with medial compartmental OA of the knee; however, no difference was found between different osteotomy techniques and no evidence is available of whether a HTO procedure could be more effective than UKR or nonoperative treatment (19). Good long-term results appear closely related to correct patient selection, accurate surgical technique and fixation, and optimal postoperative management.
The majority of the studies that have documented the survival rate of HTO used the insertion of a TKR as the end point; prognostic factors for survival are rarely investigated (3). The 10-year survival rates for HTO were reported from 51% by Naudie et al. to 93.2% by Koshimo et al. (12,33). The survival rate of HTO to treat symptomatic medial compartment OA as reported by Laprade was of 94% at 3.6 years postoperatively (17). Coventry, Ilstrup and Wallrichs recorded a survival rate of 87% at 5 years and 66% at 10 years; clinical results showed significant improvements in the mean modified Cincinnati Knee Score (from 42.9 to 65.1) and in the International Knee Documentation Committee scores both for effusions and for the single-leg hop test (34). Ekhtiari et al. documented a high propensity to return to work and sport for patients treated by HTO. Averaged across all types of HTO, more than 80% of patients returned to work, mainly by 1 year postoperatively; more physically demanding jobs required a longer time away from work. Approximately two-thirds of patients returned to work at a level of physical demand equal to or greater than their preoperative level. Moreover, approximately 80% of patients returned to sport at a level equal to or greater than their preoperative level (35).
Looking at tibial deformity, Bonnin and Chambat highlighted TBVA as an important prognostic factor. HTO has curative meaning in patients with an abnormal TBVA (>5°), because the procedure can correct the developmental deformity in these patients and normalize the obliquity of the joint line, while it has a palliative meaning in patients with a normal TBVA (<5°) (36). Many other Authors consider a TBVA (>5°) an important predictor for long-term success of the procedure. In pure degenerative intraarticular varus type of medial OA, extraarticular valgus correction is largely contraindicated, as it would lead to a pathological obliquity at the joint line (medial proximal tibial angle, MPTA >93°), which usually is correlated with fair clinical results (27). Babis et al. also looked at the obliquity of the joint line as a prognostic factor; in a series of patients with large varus deformities and OA of the medial compartment, they demonstrated in a computer model that the normal obliquity of the joint line in several cases could be preserved only with a double procedure combining a distal femoral with a proximal tibial osteotomy, without loss of ligament tension. They concluded that preservation of obliquity of the joint line within narrow boundaries of 0° was the key to success, with a 96% survival rate at a mean follow-up of 82.7 months (37). Comparable findings have been confirmed in a more recent short-term follow-up study by Hofmann and van Heerwaarden (38).
Other major positive prognostic factors include age <50 years, excellent preoperative Knee Society Score and Ahlback grade 0 arthritis of medial plateau; negative prognostic factors include obesity, especially more than 1.3 times of the normal population weight, smokers, anatomical valgus alignment of ≤5° at five weeks post operation, postoperative flexion <120°, and age >56 years old (34,39,40). Coventry, Ilstrup and Wallrichs found a lower survival rate in patients who were obese (51% vs 91%) (34). Akizuki et al. found that a BMI >27.5 is associated with early failure of the osteotomy (41). On the contrary, patients with BMI <25 showed also bad results: the hypothesis is that lighter patients are often more active, impressing a higher stress in the osteotomy site (12). Hence, patients with BMI between 25 and 27.5 showed the best results.
Niemeyer et al., in a series of 69 patients with a minimum of 36-month follow-up after MOW HTO, found that the severity of medial plateau cartilage defect did not affect the clinical results of surgery, and even partial thickness defect in lateral tibial plateau was well-tolerated (42).
There is a consensus in the literature that the loading axis in the varus malaligned osteoarthritic knees should be shifted from the varus into a slightly valgus axis; undercorrection with persisting varus usually leads to poor results, as overcorrection into large valgus may result in medial joint opening and rapid development of lateral OA. However, different opinions can be actually found on the precise amount of the valgus alignment achieved postoperatively (43). Some authors take the anatomical axis of the femur and tibia as reference and recommend a valgus of 8° to 10° postoperatively (33), others focus on the mechanical axis of the femur and tibia and suggest 3° to 5° of valgus (44). Conventry et al. reported a 10-year survival rate of 63% in knees with 5° valgus anatomical axis, 87% in knees with 6–7° valgus anatomical axis, and 94% in knees with ≥8° valgus anatomical axis (34). Fujisawa sustained that the best clinical results can be expected if the postoperative loading axis is somewhere in the range of 30% of the distance from the midpoint of the knee to the lateral joint border (45). Other clinical papers concluded that in an ideal correction, the mechanical axis should intersect the knee joint line at 62% (tolerance 60–70%) of the tibial plateau width when measured from the medial cortex, which appears to correspond to a tolerance level ±1° from the desired weight-bearing mechanical axis (4,43).
Results in osteochondritis dissecans and in osteonecrosis of the medial compartment demonstrated a significant healing response in the lesions after the affected compartment is unloaded, being the HTO the ideal base for biological reconstruction of osteochondral and chondral defects in a malaligned knee (27).
The complications of HTO can be typically subcategorised into problems specifically related to the procedure and general complications of surgery (infection, scar, deep vein thrombosis etc.); HTO entails a low serious complication rate but relatively high overall minor complication rate. Woodacre described an overall complication rate of 31%, with an overall non-union rate of 4.3% among different implants used for fixation, all subsequently revised with later successful union achieved. The infection rate requiring hospital admission was 3.5%, with a further 9.5% receiving community treatment with oral antibiotics for minor wound infections. Implant type appeared to affect non-union rates, with a lower rate in the locking compression titanium plate group (3.6% vs 8.3%), but this was not significant (5). The incidence of nonunion after HTO has been reported by other authors between 0.7% and 4.4% (46); the described risk factors for nonunion include large degree of correction in MOW HTO, smoking and insufficient fixation (47). In the past, long-term cast immobilization was unavoidable after LCW HTO, as a result patella baja secondary to patellar tendon contracture has been described with a prevalence of 7.6–8.8%. The incidence of common peroneal nerve palsy caused by nerve damage during LCW HTO has been described in 2–16% of cases, and fibular shaft osteotomy has been suggested for reduction of such damage. The reported rate of infection following external fixation is 2.3–54.5%, whereas that of infection following internal fixation is ≤4%. Other reported complications include fixation failure, loss of correction, pseudoarthrosis, deep venous thrombosis, pulmonary embolism, and compartment syndrome (9).
Conclusions
HTO has been historically intended as a definitive treatment strategy for medial compartment knee OA; after a period in which it felt out of favour due to the diffusion of TKR and UKR, it has more recently been reappreciated. Its main indication remains the correction of varus malalignment in medial unicompartmental knee OA in young and active patients, and the 2005 ISAKOS protocol is even now highly accepted to define ideal patients, possible patients and patients not suitable for tibial osteotomy. Furthermore, a second indication of HTO is the treatment of ligament deficient knees: altering the tibial slope, the HTO can increase stability in ACL and PCL insufficiency. The tibial slope should be increased in PCL deficiency and increased in ACL deficiency; moreover, HTO can increase knee stability in chronic PLC deficiency reducing the varus thrust. Lastly, HTO can even be intended as an adjunctive or isolated treatment for meniscal, chondral and osteochondral pathologies, since the procedure proved a significant healing response.
There is a consensus that the loading axis in the varus osteoarthritic knee should be shifted into a slightly valgus axis; however, different opinions can be found on the precise amount of the valgus alignment which must be achieved postoperatively. The two most commonly used surgical techniques for HTO are the LCW and the MOW. While the LCW was largely used in past years, the MOW has more recently had a growing diffusion due to the development of more stable implants and to some technical modifications like the introduction of the biplanar osteotomy. However, no high grade evidence is available as to whether LCW or MOW is more effective in the treatment of symptomatic medial knee OA. Patellar height and tibial slope changes are two major concerns in HTO. Regarding patellar height, some authors suggest a MOW with a patella alta and a LCW with a patella baja; nevertheless, only an associated tibial tubercle osteotomy permits the complete avoidance of patellar height change or its precise correction. Tibial slope changes can be avoided by assiduous attention to surgical technique instead. Several solutions have been used to fill the MOW osteotomy gap: bone autograft is still considered the gold standard, but modern fixation implants often consent to leave the gap unfilled.
Regarding reported clinical results, HTO has generally proven to be an effective procedure reducing pain and improving knee function in patients with medial knee OA. Good long-term results are usually related to correct patient selection, careful surgical technique and accurate fixation. In the literature, 10-year survival rates of HTO is reported up to 93%; moreover, high propensity to return to work and sport activities after HTO has been reported, around 80%.
As reported by the literature, good prognostic factors for long-term success of the procedure turned out to be the presence of a metaphyseal varus with an abnormal TBVA (>5°), the preservation of the normal obliquity of the joint line, age <50 years, excellent preoperative Knee Society Score, Ahlback grade 0 arthritis of medial tibial plateau, BMI between 25–27.5. Bad prognostic factors are obesity with BMI >27.5, heavy smoking, insufficient correction of varus, low postoperative flexion and age >56 years old.
Possible complications related to HTO are non-union, infection, patella baja secondary to patellar tendon contracture, common peroneal nerve palsy (in LCW), fixation failure, loss of correction and other general complications of surgery such as deep venous thrombosis, pulmonary embolism and compartment syndrome. In spite of a relatively high overall minor complication rate, HTO revealed a low serious complication rate.
In conclusion, HTO can be currently considered a safe and effective procedure; its growing appreciation is due to the stepwise advances in the surgical technique and the fixation devices as well as to the progression of sports medicine, soft tissue and chondral surgery. Based on its clinical results, HTO is nowadays widely accepted as a preferred alternative to a knee arthroplasty in young patients with medial degenerative changes in a varus knee, particularly in active population or physically demanding workers.
Acknowledgments
Funding: None.
Footnote
Provenance and Peer Review: This article was commissioned by the Guest Editor (Luigi Sabatini) for the series “Osteotomies and partial replacement in early osteoarthritis of the knee” published in Annals of Joint. The article has undergone external peer review.
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/aoj.2017.06.06). The series “Osteotomies and partial replacement in early osteoarthritis of the knee” was commissioned by the editorial office without any funding or sponsorship. The authors have no other conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Gomoll AH, Angele P, Condello V, et al. Load distribution in early osteoarthritis. Knee Surg Sports Traumatol Arthrosc 2016;24:1815-25. [Crossref] [PubMed]
- Debeyre J, Patte D. Value of corrective osteomies in the treatment of certain knee diseases with axial deviation. Rev. Rhum Mal Osteoartic 1962;29:722-9. [PubMed]
- Brinkman JM, Lobenhoffer P, Agneskirchner JD, et al. Osteotomies around the knee: patient selection, stability of fixation and bone healing in high tibial ostetomies. J Bone Joint Surg Br 2008;90:1548-57. [Crossref] [PubMed]
- Sabzevari S, Ebrahimpour A, Khalilipour Roudi M, et al. High tibial osteotomy: a sistematic review and current concept. Arch Bone Jt Surg 2016;4:204-12. [PubMed]
- Woodacre T, Ricketts M, Evans JT, et al. Complication associated with opening wedge high tibial osteotomy- A review of the literature and 15 years of experience. Knee 2016;23:276-82. [Crossref] [PubMed]
- Noyes FR, Barber SD, Simon R. High tibial osteotomy and ligament reconstruction in varus angulated, anterior cruciate ligament-deficient knees: a two to seven year follow up study. Am J Sports Med 1993;21:2-12. [Crossref] [PubMed]
- Thompson SR, Zabtia N, Weening B, et al. Arthroscopic and computer-assisted high tibial osteotomy using standard total knee arthroplasty navigation software. Arthrosc Tech 2013;2:e161-6. [Crossref] [PubMed]
- Rand JA, Neyret P. ISAKOS meeting on the management of osteoarthritis of the knee prior to total knee arthroplasty. Lyon, France: ISAKOS Congress; 2005.
- Lee DC, Byun SJ. High Tibial Osteotomy. Knee Surg Relat Res 2012;24:61-9. [Crossref] [PubMed]
- Chahla J, Dean CS, Mitchell JJ, et al. Medial Opening Wedge Proximal Tibial Osteotomy. Arthrosc Tech 2016;5:e919-28. [Crossref] [PubMed]
- Flecher X, Parratte S, Aubaniac JM, et al. A 12-28-year followup study of closing wedge high tibial osteotomy. Clin Orthop Relat Res 2006;91-6. [Crossref] [PubMed]
- Naudie D, Bourne RB, Rorabeck CH, et al. The Install Award. Survivorship of the high tibial valgus osteotomy. A 10- to -22-year followup study. Clin Orthop Relat Res 1999;18-27. [PubMed]
- . Arch Orthop Trauma Surg. Long-term outcome after high tibial osteotomy. Arch Orthop Trauma Surg 2008;128:345-5. [Crossref]
- Rudan JF, Simurda MA. High tibial osteotomy. A prospective clinical and roentgenographic review. Clin Orthop Relat Res 1990;251-6. [PubMed]
- Stuchin SA, Johanson NA, Lachiewicz PF, et al. Surgical management of inflammatory arthritis of the adult hip and knee. Instr Course Lect 1999;48:93-109. [PubMed]
- Prodromos CC, Amendola A, Jakob RP. High tibial osteotomy: indications, techniques, an postoperative management. Instr Course Lect. 2015;64:555-65. [PubMed]
- Laprade RF, Spiridonov SI, Nystrom LM, et al. Prospective outcomes of young and middle-aged adults with medial compartment osteoarthritis treated with a proximal tibial opening wedge osteotomy. Arthroscopy 2012;28:354-64. [Crossref] [PubMed]
- Lobenhoffer P, Agneskirchner JD. Improvements in surgical technique of valgus high tibial osteotomy. Knee Surg Sports Traumatol Arthrosc 2003;11:132-8. [Crossref] [PubMed]
- Brouwer RW, Huizinga MR, Duivenvoorden T, et al. Osteotomy for treating knee osteoarthritis. Cochrane Database Syst Rev 2014;12:CD004019 [PubMed]
- Huizinga MR, Brouwer RW, van Raaij TM. High tibial osteotomy: closed wedge versus combined wedge osteotomy. BMC Musculoskelet Disord 2014;15:124. [Crossref] [PubMed]
- Portner O. High Tibial Osteotomy and Patellar Height: Closing, Opening or Combined? Patellar Height as a Determining Factor. Clin Orthop Relat Res 2014;472:3432-40. [Crossref] [PubMed]
- Staubli AE, Jacob HA. Evolution of open-wedge high-tibial osteotomy: experience with a special angular stable device for internal fixation without interposition material. Int Orthop 2010;34:167-72. [Crossref] [PubMed]
- Song SJ, Bae DK. Computer-assisted navigation in high tibial osteotomy. Clinics in Orthopedic Surgery 2016;8:349-57. [Crossref] [PubMed]
- Giffin JR, Vogrin TM, Zantop T, et al. Effects of increasing tibial slope on the biomechanics of the knee. Am J Sports Med 2004;32:376-82. [Crossref] [PubMed]
- Dean CS, Liechti DJ, Chahla J, et al. Clinical Outcomes of high tibial osteotomy for knee instability. Orthop J Sports Med 2016;4:2325967116633419 [Crossref] [PubMed]
- Smith TO, Sexton D, Mitchell P, et al. Opening- or closing-wedged high tibial osteotomy: a meta-analysis of clinical and radiological outcomes. Knee 2011;18:361-8. [Crossref] [PubMed]
- Lobenhoffer P. The role of high tibial osteotomy. Florence: The osteoathritic knee. The 2nd Best Current Practice in Europe (BCPE); 2013: 9.
- Magnussen RA, Dahm DL, Neyret P. Osteotomy for slope correction following failed ACL reconstruction. In: Marx RG. editors. Revision ACL Reconstruction. New York: Springer New York, 2014:221-6.
- Herman BV, Giffin JR. High tibial osteotomy in the ACL-deficient knee with medial compartment osteoarthritis. J Orthop Traumatol 2016;17:277-85. [Crossref] [PubMed]
- Naudie DD, Amendola A, Fowler PJ. Opening wedge high tibial osteotomy for symptomatic hyperextension-varus thrust. Am J Sports Med 2004;32:60-70. [Crossref] [PubMed]
- Phisitkul P, Wolf BR, Amendola A. Role of high tibial and distal femoral osteotomies in the treatment of lateral-posterolateral and medial instabilities of the knee. Sports Med Arthrosc 2006;14:96-104. [Crossref] [PubMed]
- Arthur A, LaPrade RF, Angel J. Proximal tibial opening wedge osteotomy as the initial treatment for chronic posterolateral corner deficiency in the varus knee: a prospective clinical study. Am J Sports Med 2007;35:1844-50. [Crossref] [PubMed]
- Koshino T, Moril J, Wada H, et al. High tibial osteotomy with fixation by a blade plate for medial compartment osteoarthritis of the knee. Orthop Clin North Am 1989;20:227-43. [PubMed]
- Coventry MB, Ilstrup DM, Wallrichs SL. Proximal tibial osteotomy: a critical longterm study of eighty-seven cases. J Bone Joint Surg Am 1993;75:196-201. [Crossref] [PubMed]
- Ekhtiari S, Haldane CE, Simunovic N. Return to Work and Sport Following High Tibial Osteotomy A Systematic Review. J Bone Joint Surg Am 2016;98:1568-77. [Crossref] [PubMed]
- Bonnin M, Chambat P. Current status of valgus angle, tibial head closing wedge osteotomy in medial gonarthrosis. Orthopade 2004;33:135-42. [Crossref] [PubMed]
- Babis GC, An KN, Chao EY, et al. Double level osteotomy of the knee: a method to retain joint-line obliquity. J Bone Joint Surg Am 2002;84-A:1380-8. [Crossref] [PubMed]
- Hofmann S, van Heerwaarden RJ. Algemeine Patientenauswahl und Indikationen zu Doppelosteotomien. Orthopädische Praxis 2007;43:142-6.
- Odenbring S, Tjörnstrand B, Egund N, et al. Function after tibial osteotomy for medial gonarthrosis below aged 50 years. Acta Orthop Scand 1989;60:527-31. [Crossref] [PubMed]
- Bonasia DE, Dettoni F, Sito G, et al. Medial opening wedge high tibial osteotomy for medial compartment overload/arthritis in the varus knee: prognostic factors. Am J Sports Med 2014;42:690-8. [Crossref] [PubMed]
- Akizuki S, Shibakawa A, Takizawa T, et al. The long-term outcome of high tibial osteotomy: a ten-to 20-year follow up. J Bone Joint Surg Br 2008;90:592-6. [Crossref] [PubMed]
- Niemeyer P, Schmal H, Hauschild O, et al. Open-wedge osteotomy using an internal plate fixator in patients with medial-compartment gonarthritis and varus malalignment: 3-year results with regard to preoperative arthroscopic and radiographic findings. Arthroscopy 2010;26:1607-16. [Crossref] [PubMed]
- Agneskirchner JD, Hurschler C, Christiane D, et al. The effects of valgus medial opening wedge high tibial osteotomy on articular cartilage pressure of the knee: a biomechanical study. Arthroscopy 2007;23:852-61. [Crossref] [PubMed]
- Hernigou P, Ovadia H, Goutallier D. Mathematical modelling of open-wedge tibial osteotomy and correction tables. Rev Chir Orthop Reparatrice Appar Mot 1992;78:258-63. [PubMed]
- Fujisawa Y, Masuhara K, Shiomi S. The effect of high tibial osteotomy on osteoarthritis of the knee. An arthroscopic study of 54 knee joints. Orthop Clin North Am 1979;10:585-608. [PubMed]
- Valkering KP, van den Bekerom MP, Kappelhoff FM, et al. Complications after Tomofix medial opening wedge high tibial osteotomy. J Knee Surg 2009;22:218-25. [Crossref] [PubMed]
- Amendola A, Bonasia DE. Results of high tibial osteotomy: review of the literature. Int Orthop 2010;34:155-60. [Crossref] [PubMed]
Cite this article as: Capella M, Gennari E, Dolfin M, Saccia F. Indications and results of high tibial osteotomy. Ann Joint 2017;2:33.


