
Primary total hip arthroplasty through a direct anterior approach using a bikini incision: surgical technique
Introduction
The direct anterior approach (DAA) for primary total hip arthroplasty (THA) has many potential advantages (1-9). Recently, a bikini type oblique incision has been proposed to improve cosmetic appearance of the surgical scar following primary THA, particularly, in the female patient population. Leunig et al. have compared the standard longitudinal DA incision (n=33 patients) with the modified bikini type incision (n=26 patients) (10). At 6 months of follow-up, patients who underwent THA through a bikini incision were more satisfied in the aesthetic appearance of the scar. Functional scores, pain, and complications were similar between the two groups. The safety of this modified bikini DAA incision has been also reported in a larger cohort of patients. One hundred patients underwent primary THAs through a bikini type incision with no reported complications related to numbness, thigh pain, component malposition, and leg length discrepancy (11). The aim of this article is to report the senior author’s (William J. Hozack) experience and surgical technique of the bikini type incision for primary THA using the DAA.
Surgical technique
Patient positioning and the operating room table set up is performed similar to the standard DAA technique, as described previously by the senior author (William J. Hozack) (12).
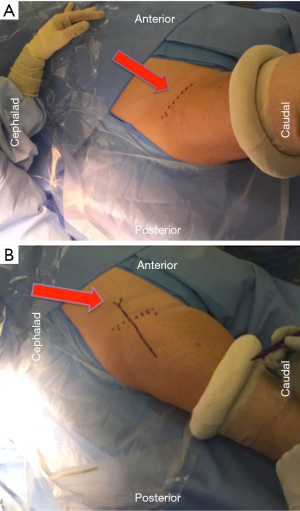
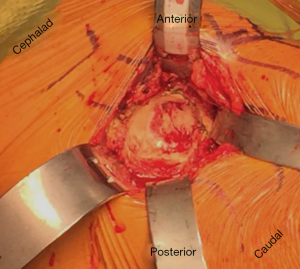
The surface anatomical landmarks start by locating the inguinal skin crease. This can be easily identified with slight hip flexion (Figure 1A). Next the anterior superior iliac spine (ASIS) is identified and marked. The center of the bikini incision is typically either on or slightly distal [1 centimeter (cm)], but parallel, to the skin crease mark with 50% of the incision length medial and 50% lateral to the ASIS (Figure 1B). Making the incision distal to the skin crease facilitates exposure of the acetabulum. However, if the distance between ASIS and skin crease is more than 3 cm, the incision will be made on the inguinal skin crease. With longitudinal superior and inferior retraction to skin, the fascial layer of tensor fascia lata (TFL) is dissected longitudinally on the lateral side of the incision (Figure 2). It is important to minimize medial superficial dissection to reduce the risk to the lateral femoral cutaneous nerve (LFCN). Once the subcutaneous dissection is complete, the remainder of the exposure proceeds in an identical fashion to that described using a longitudinal incision (12). It is critical then to confirm the location of TFL. One method to recognize the muscle is visualizing the perforating vessels that enter at the mid portion of TFL. Another method to determine the TFL location is to proximally palpate the ASIS and confirm that the TFL is lateral to it. Once the muscular interval has been identified (between TFL and sartorius), an assessment of incision length and exposure is performed for potential extension laterally or medially. Small increments in incision length can substantially change the ease of exposure of the deep structures. This is followed by a longitudinal incision through the superficial fascia of the TFL muscle in line with the muscle fibers (Figure 3). A deep blunt dissection is then made similar to the standard DA technique and followed by ligation of the ascending branches of lateral circumflex artery. The capsule of the hip joint is carefully exposed using specifically designed retractors. Gentle release of the reflected head of the rectus aids in improving exposure. Next, an anterior capsulectomy is preformed, which improves the ease of exposure of both the femur and acetabulum. The femoral neck is then cut in situ (napkin ring fashion) with an oscillating saw, and the femoral head is removed. Three acetabular retractors are placed (anterior, posterior and inferior) to obtain optimal acetabular exposure (Figure 4). Reaming is performed in the standard fashion. Occasionally offset acetabular reamers are used to facilitate accomplishing this step without excessive skin retraction (Figure 5). The cup is then inserted using an offset insertion handle. The polyethylene liner is placed by hand.


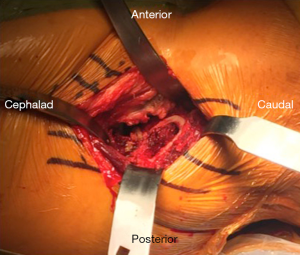
Femoral exposure is identical to our standard DAA technique. First the femur is externally rotated 90 degrees to allow elevation (Figure 6). With proper retractor placement, the superior capsule can be identified and partially excised. Subsequently, a superolateral double-tipped retractor is placed over the top of the greater trochanter. Additional superior capsular release is performed, and the femur is then elevated using a bone hook with the retractor holding the femur in place. The limb is then repositioned into external rotation and adduction with the knee extended. This allows for proper access to the femur for broaching and implant insertion (Figure 7). Before broaching the femur, distal skin retraction can be used to improve visualization (Figure 8). An offset broach handle is used to achieve safe broaching and seating of the femoral stem (Figure 9). Once the final components are placed and the hip stability, range of motion, and leg length discrepancy is checked, closure is performed in the standard fashion. Care is taken to not entwine the LCFN during the subcutaneous closure.


Preliminary results
A total of 79 patients underwent THAs through a DAA using a bikini incision performed by the senior author (William J. Hozack). There were 70 females (89%) and 9 males (11%) with an average age of 62 years. The available follow-up period ranged between 1 and 7 months postoperatively. All patients were satisfied with the cosmetic appearance of the incision (Figure 10) with no reported complications.

Summary
In addition to the reported advantages of DAA in THA, the preliminary results of the bikini type incision have proven the safety while improving the cosmetic appearance of the surgical scar. To protect the LCFN during this technique, minimal medial superficial dissection and careful superficial closure should be emphasized. The important keys to the acetabular and femoral preparation and exposure are retractor placement and use of offset instruments when needed to ensure safe preparation and satisfactory seating of the final implants.
Acknowledgments
Funding: None.
Footnote
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/aoj.2017.03.01). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Helsinki Declaration (as revised in 2013). Written informed consent was obtained from the patient for publication of this manuscript and any accompanying images.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Berend KR, Lombardi AV Jr, Seng BE, et al. Enhanced early outcomes with the anterior supine intermuscular approach in primary total hip arthroplasty. J Bone Joint Surg Am 2009;91:107-20. [Crossref] [PubMed]
- Bergin PF, Doppelt JD, Kephart CJ, et al. Comparison of minimally invasive direct anterior versus posterior total hip arthroplasty based on inflammation and muscle damage markers. J Bone Joint Surg Am 2011;93:1392-8. [Crossref] [PubMed]
- Bremer AK, Kalberer F, Pfirrmann CW, et al. Soft-tissue changes in hip abductor muscles and tendons after total hip replacement: comparison between the direct anterior and the transgluteal approaches. J Bone Joint Surg Br 2011;93:886-9. [Crossref] [PubMed]
- Meneghini RM, Pagnano MW, Trousdale RT, et al. Muscle damage during MIS total hip arthroplasty: Smith-Petersen versus posterior approach. Clin Orthop Relat Res 2006;293-8. [Crossref] [PubMed]
- Goebel S, Steinert AF, Schillinger J, et al. Reduced postoperative pain in total hip arthroplasty after minimal-invasive anterior approach. Int Orthop 2012;36:491-8. [Crossref] [PubMed]
- Martin CT, Pugely AJ, Gao Y, et al. A comparison of hospital length of stay and short-term morbidity between the anterior and the posterior approaches to total hip arthroplasty. J Arthroplasty 2013;28:849-54. [Crossref] [PubMed]
- Poehling-Monaghan KL, Kamath AF, Taunton MJ, et al. Direct anterior versus miniposterior THA with the same advanced perioperative protocols: surprising early clinical results. Clin Orthop Relat Res 2015;473:623-31. [Crossref] [PubMed]
- Restrepo C, Parvizi J, Pour AE, et al. Prospective randomized study of two surgical approaches for total hip arthroplasty. J Arthroplasty 2010;25:671-9.e1. [Crossref] [PubMed]
- Taunton MJ, Mason JB, Odum SM, et al. Direct anterior total hip arthroplasty yields more rapid voluntary cessation of all walking aids: a prospective, randomized clinical trial. J Arthroplasty 2014;29:169-72. [Crossref] [PubMed]
- Leunig M, Faas M, von Knoch F, et al. Skin crease 'bikini' incision for anterior approach total hip arthroplasty: surgical technique and preliminary results. Clin Orthop Relat Res 2013;471:2245-52. [Crossref] [PubMed]
- Nizam I. The Bikini Hip Replacement - Surgical Technique Preserving Vessels and Deep Soft Tissues in Direct Anterior Approach Hip Replacement. J Orthop Res Physiother 2015;1:007.
- Post ZD, Orozco F, Diaz-Ledezma C, et al. Direct anterior approach for total hip arthroplasty: indications, technique, and results. J Am Acad Orthop Surg 2014;22:595-603. [Crossref] [PubMed]
Cite this article as: Makhdom AM, Goel R, Hozack WJ. Primary total hip arthroplasty through a direct anterior approach using a bikini incision: surgical technique. Ann Joint 2017;2:10.




