
Comparison of patient-specific instruments with the computer-assisted navigation in total knee arthroplasty for osteoarthritis in a patient with femoral fracture malunion
Introduction
Alignment deviation of the lower limb resulting from posttraumatic deformity of femur can cause knee osteoarthritis. Restoring proper limb alignment through intra-articular resection and soft tissue balancing in total knee arthroplasty (TKA) has been described as management of these cases (1). Extra-articular femoral deformity makes accuracy resection difficult because the conventional devices guiding resection may be inapplicable (2). The intramedullary (IM) device is used commonly for the distal femoral bone cut and most surgeons find the IM devices are reproducible and easy in the majority of cases (3). However, for a femur with traumatic deformity, the marrow cavity may be irregular or blocked and the anatomical valgus angle is abnormal. In this situation, resection following the IM guide may cause an unacceptable deviation. It may be associated with higher incidence of aseptic loosening, abnormal polyethylene wear and other complications (4,5).
A variety of new TKA instruments have sprung up to overcome the weakness of the conventional devices in the complex TKA including extramedullary devices, computer-assisted navigation (CAN) and patient-specific instruments (PSI) (1,6,7). PSI was introduced as a new technique in recent years to achieve the same accuracy of navigation and avoid high cost and long operation time (8). In this report, the PSI and a portable CAN were applied to guide coronal resection in TKA. We discussed the accuracy and maneuverability of these two devices and made an objective appraisal.
Case presentation
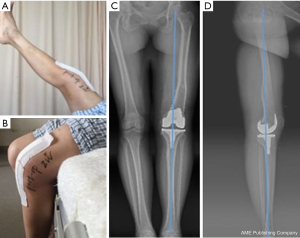
A 58-year-old female patient complaining of a left knee pain for over 10 years presented to our clinic in August 2016. She encountered a fracture of left femoral shaft about 40 years ago. Inappropriate nonsurgical treatment resulted in the femur deformity and lower limb shortening. Physical examination showed a 15 degrees’ mild left genu varum. Fixed flexion deformity (FFD) of the left knee was observed. Active range of motion was 10 to 40 degrees.
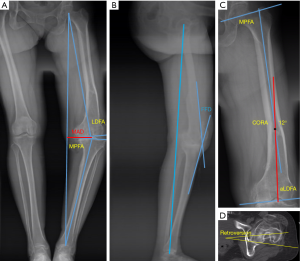
The Kellgren-Lawrence grade IV osteoarthritic change of the left knee was documented. Weight bearing X-ray (Figure 1A) showed malunion of the left femoral shaft fracture. The hip-knee-ankle (HKA) angle is 155 degrees. Mechanical lateral distal femoral angle (LDFA) was 99 degrees. There was 20 degrees’ FFD on the sagittal view (Figure 1B). The center of rotation of angulation (CORA) of the femur was 12 degrees (Figure 1C). There was neither multiapical angular deformity nor a translation deformity. Computed tomography (CT) of the femur (Figure 1D) showed external rotational deformity of the femur shaft.
Given her age and the severe symptoms, we finally decided to perform TKA for her left knee. For patients with extra-articular deformity and arthritis of the knee, one-stage TKA or two stage extra-articular corrective osteotomy and TKA have been considered (9). As described in the previous studies (10), the greater and the farther away from the joint the angular deformity is, the more likely extra-deformity correction is needed. The femoral angular deformity of this case was not so severe and we found the attachment of lateral collateral ligament was safe when planning the distal femoral resection preoperatively. Extra-articular osteotomy was not necessary and TKA combined with intra-articular resection was an ideal management.
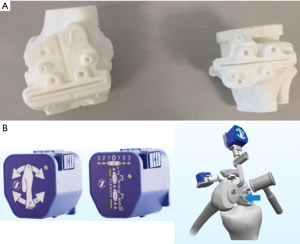
The femoral extra-articular deformity made the IM device inapplicable. To solve this problem, the surgeon planned to use the PSI and CAN. For the PSI, the personal skeleton model and the cutting guides were manufactured by Beijing AKEC Medical Co. through 3-D printing according to the CT and 3-D reconstruction of the full leg (Figure 2A). The CAN we selected was iASSIST Knee promoted by Zimmer recently (Figure 2B). The operation was performed in August 2016. Two weeks later, there was no pain at her left knee and she could walk unaided. Active range of motion was 0 to 100 degrees. The postoperative standing scanogram (Figure 3) showed favorable limb alignment.
Surgery technique
The surgery was performed through an anterior longitudinal incision and a medial parapatellar approach. The cruciate ligaments, hyperplastic osteophyte or soft tissue were cleared and the contractive ligaments were released properly to provide adequate visualization for the following resection.
The PSI was used to guide the distal femoral resection initially (Figure 4A). The cartilage or other soft tissue must be scraped off the cortical bone. The cutting guide was located on the distal femur through three bone landmarks which are determined on the surface of the skeleton model in advance. The thickness of the resection was 9 mm. There was only one gap on the cutting guide and it couldn’t be shift to change the thickness of resection.
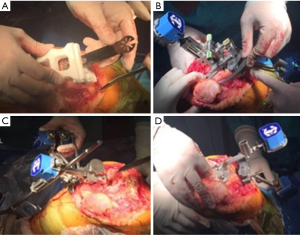
Then the PSI was removed and the iASSIST Knee was used. A short rod and several headed pins help fix the sensors and the cutting guide on the distal femur (Figure 4B). The surgeon put the hip in 13 random positions around the rotation center. The navigation system calculated the hip rotation center and femur mechanical axis. Under the guide of the navigation, the resected surface was perpendicular to the mechanical axis. The primary thickness of the resection was 9 mm and the surgeon could add the thickness by 4 mm mostly. After resection, the surgeon verified the accuracy of resection and adjusted it timely through navigation. This is the distinct advantage of CAN. The tibial mechanical axis was determined by the navigation system with the help of ankle center and the tibial intercondylar eminence. The cutting guide was fixed perpendicularly to the mechanical axis on the coronal plane with a 3-degree of slope (Figure 4C). After resection, the verification is similar to the distal femoral resection (Figure 4D).
Through the gap balance technique, the 4-in-1 cutting guide was used to perform the femoral anteroposterior (AP) resection. The flexion and extension gap are almost equal and there was no anterior notching or overstuff of the femur. After irrigation thoroughly, the cement components and the polymethylene insert were implanted. The tension of the bilateral joint gaps was moderate. The varus deformity was corrected and the range of motion after suture was 0 to 160 degrees.
Discussion
It is technically difficult to perform accurate distal femoral resection with conventional IM devices in the presence of femoral extra-articular deformity (1,2). PSI and CAN are both alternatives and many studies compared them with conventional devices in normal TKA with different conclusions (11-14). However, few studies did this in TKA with extra-articular deformity, because conventional devices don’t apply for these cases. PSI and CAN have unique advantage in managing complicated TKA.
In terms of preoperative preparation, PSI is more cumbersome. The CT and 3-D reconstruction of the full leg are needed to help design the PSI, which will spend another 5 to 7 days. In addition, the printed PSI must be sterilized in advance. Respectively, iASSIST Knee is convenient except the intraoperative registration for about 15 minutes.
The PSI is located according to three bone landmarks determined in advance. This method of fixation may be inaccurate and sometimes the cutting guide can’t match the osseous surface completely. The soft tissue or cartilage must be scraped off because they can’t be visualized on CT. How accurate can bony landmarks be determined on CT is a question (15). Some other PSI are based on magnetic resonance imaging (13), which may avoid this problem. For the iASSIST Knee, the navigation catches the rotation center of the hip and finds the mechanical axis as the femur moves randomly around the hip. Under the guide of navigation, the surgeon can tune the resected surface timely to keep the deviation within 1 degree. It seems CAN is more reliable and accurate than the PSI. This outcome is similar to the previous studies in normal TKA (16).
Bali et al. reported that the mean blood loss and skin-to-skin time were shorten in TKA with PSI (17). The surgeon can finish the resection just through the cutting guides and the instruments involved are less than conventional devices and CAN. While Hamilton et al. found the PSI doesn’t shorten the surgery time (18). The cutting guide of PSI has only one resection gap and the surgeon can’t tune the resection thickness by the PSI as the cutting guide has only one resection gap. The conventional devices are needed in this situation, which may increase the operation time. For CAN, installation of the instruments and determination of resection surface demand much more time. The complex intraoperative procedure is an important weakness of CAN.
Overall, the accurate resection is important to re-establish the neutral alignment deviation of the lower limb. The patient in this case demonstrated a satisfactory functional outcome and good lower limb alignment. The PSI and CAN with different characteristics are alternatives in complicated TKA with extra-articular deformity.
Acknowledgments
Funding: None.
Footnote
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/aoj.2016.12.01). QJ serves as an Editor-in-Chief of Annals of Joint from Mar 2016 to Feb 2021. DS serves as an unpaid Executive Editor-in-Chief of Annals of Joint from Mar 2016 to Feb 2021. The other authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Helsinki Declaration (as revised in 2013). The patient in this case report has given her informed consent for the case report to be published.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Wang JW, Wang CJ. Total knee arthroplasty for arthritis of the knee with extra-articular deformity. J Bone Joint Surg Am 2002;84-A:1769-74. [Crossref] [PubMed]
- Papagelopoulos PJ, Karachalios T, Themistocleous GS, et al. Total knee arthroplasty in patients with pre-existing fracture deformity. Orthopedics 2007;30:373-8. [PubMed]
- Dennis DA, Channer M, Susman MH, et al. Intramedullary versus extramedullary tibial alignment systems in total knee arthroplasty. J Arthroplasty 1993;8:43-7. [Crossref] [PubMed]
- Moreland JR. Mechanisms of failure in total knee arthroplasty. Clin Orthop Relat Res 1988;49-64. [PubMed]
- Wasielewski RC, Galante JO, Leighty RM, et al. Wear patterns on retrieved polyethylene tibial inserts and their relationship to technical considerations during total knee arthroplasty. Clin Orthop Relat Res 1994;31-43. [PubMed]
- Fehring TK, Mason JB, Moskal J, et al. When computer-assisted knee replacement is the best alternative. Clin Orthop Relat Res 2006;132-6. [Crossref] [PubMed]
- Huijbregts HJ, Khan RJ, Fick DP, et al. Component alignment and clinical outcome following total knee arthroplasty: a randomised controlled trial comparing an intramedullary alignment system with patient-specific instrumentation. Bone Joint J 2016;98-B:1043-9. [Crossref] [PubMed]
- Conteduca F, Iorio R, Mazza D, et al. Patient-specific instruments in total knee arthroplasty. Int Orthop 2014;38:259-65. [Crossref] [PubMed]
- Lonner JH, Siliski JM, Lotke PA. Simultaneous femoral osteotomy and total knee arthroplasty for treatment of osteoarthritis associated with severe extra-articular deformity. J Bone Joint Surg Am 2000;82:342-8. [Crossref] [PubMed]
- Mullaji A, Shetty GM. Computer-assisted total knee arthroplasty for arthritis with extra-articular deformity. J Arthroplasty 2009;24:1164-9.e1. [Crossref] [PubMed]
- Hoffart HE, Langenstein E, Vasak N. A prospective study comparing the functional outcome of computer-assisted and conventional total knee replacement. J Bone Joint Surg Br 2012;94:194-9. [Crossref] [PubMed]
- Lee GC. Patient specific instrumentation. J Arthroplasty 2015;30:719-20. [Crossref] [PubMed]
- Ng VY, DeClaire JH, Berend KR, et al. Improved accuracy of alignment with patient-specific positioning guides compared with manual instrumentation in TKA. Clin Orthop Relat Res 2012;470:99-107. [Crossref] [PubMed]
- Anderson KC, Buehler KC, Markel DC. Computer assisted navigation in total knee arthroplasty: comparison with conventional methods. J Arthroplasty 2005;20:132-8. [Crossref] [PubMed]
- Victor J, Van Doninck D, Labey L, et al. How precise can bony landmarks be determined on a CT scan of the knee? Knee 2009;16:358-65. [Crossref] [PubMed]
- Lustig S, Scholes CJ, Oussedik SI, et al. Unsatisfactory accuracy as determined by computer navigation of VISIONAIRE patient-specific instrumentation for total knee arthroplasty. J Arthroplasty 2013;28:469-73. [Crossref] [PubMed]
- Bali K, Walker P, Bruce W. Custom-fit total knee arthroplasty: our initial experience in 32 knees. J Arthroplasty 2012;27:1149-54. [Crossref] [PubMed]
- Hamilton WG, Parks NL, Saxena A. Patient-specific instrumentation does not shorten surgical time: a prospective, randomized trial. J Arthroplasty 2013;28:96-100. [Crossref] [PubMed]
Cite this article as: Yao C, Xu X, Jiang Q, Shi D. Comparison of patient-specific instruments with the computer-assisted navigation in total knee arthroplasty for osteoarthritis in a patient with femoral fracture malunion. Ann Joint 2017;2:2.


