Orthopaedic sports injuries in youth: the hip
Pediatric HIP disorders
Hip injuries in the pediatric athlete have become more common as overall participation in organized, competitive youth sports has increased over the past decades (1,2). Improved diagnostic imaging studies and utilization of hip arthroscopy in the pediatric setting have also led to the increased diagnosis of hip injuries (3). These hip disorders can be classified as either acute injuries or chronic, overuse injuries. This chapter will focus on the most common acute and chronic injuries to the hip in the pediatric patient.
Apophyseal avulsion fractures
Epidemiology
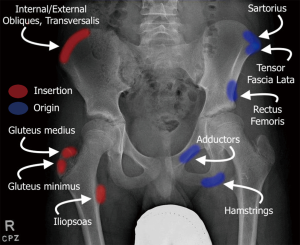
Apophyseal avulsion fractures are generally atraumatic and occur when there is a sudden eccentric contraction or passive stretch of muscle such as in exercises involving sprinting, jumping, and/or kicking. The Sharpey’s fibers attaching from the muscle/tendon unit onto the epiphysis are stronger than the cells in the physis, resulting in failure through the zone of hypertrophy of the physis (4). These injuries can occur at any major muscle attachment site. The most common areas in the hip and pelvis are the anterior superior iliac spine (ASIS), anterior inferior iliac spine (AIIS), ischial tuberosity, lesser trochanter, and iliac crest. Reports vary on the incidence of each type of avulsion fracture (Figure 1) (5,6). Schuett et al. most recently reported on 228 patients with apophyseal avulsion fractures, with 49% of avulsions occurring at the AIIS and 30% occurring at the ASIS (7). In contrast, Metzmaker et al. found that ASIS avulsion fractures (40%) were the most predominant in their cohort (5). Rossi et al. reported that ischial tuberosity fractures encompassed 53% of the avulsion injuries reported (6). It is postulated that the differences in climate where the studies were conducted, differing regimens of youth athlete stretching and warm-up, and the level of competitiveness of the athletes in each cohort may have contributed to the differences in incidence of types of avulsion fractures between the studies.
History and physical exam
Apophyseal avulsion injuries typically present with a sudden forceful, atraumatic movement followed by acute sharp pain at the site of injury. Pain is worse with activity and improves with rest. Patients may also complain of associated weakness. On physical exam, the patient presents with guarding with the extremity held in a position of least muscle-tendon tension. There will be tenderness to palpation at the apophysis with possible swelling and bruising. Active activation or passive stretch of the muscle/tendon group will lead to pain.
Imaging
AP pelvis radiograph should be obtained that generally shows an avulsion fracture (7). If negative, then additional oblique views of the pelvis can be obtained to better delineate a subtle fracture. Adolescents with hip pain should include AP and frog leg lateral radiographs of the hip to rule out SCFE (slipped capital femoral epiphysis). Non-displaced avulsion fractures may be difficult to visualize so advanced imaging such as MRI can be used to help diagnose these injuries. Ultrasound can also be used with the benefit of dynamic examination and no radiation exposure (8).
Treatment
The vast majority of apophyseal avulsion injuries are successfully treated non-operatively. Patients are encouraged to rest, ice, and use anti-inflammatories as needed for the first week after initial injury. Crutches may be useful to promote a normal gait pattern during recovery. Activity is then gradually increased with allowance of gentle stretching followed by resistance training, sport specific training, and eventual return to sport (6,9).
In certain instances, non-operative treatment fails. Schuett et al. reported 98% of patients improved with non-operative management. However, pain greater than 3 months from the initial injury was present in 14% of their cohort. AIIS avulsion fractures were more than 4 times more likely to have chronic pain, possibly secondary to an associated hip labral injury. Operative treatment may be recommended for fracture displacement at initial injury greater than 2 cm given the increased risk of nonunion and chronic pain (5,7).
Coxa saltans
Epidemiology
Coxa saltans, also known as snapping hip syndrome, is characterized by a snapping sensation in the hip, commonly occurring in athletes. There are two main types: extra-articular (includes external and internal subtypes) and intra-articular. The most commonly encountered form is the external subtype of extra-articular snapping hip syndrome. External snapping hip is caused by the posterior iliotibial (IT) band or anterior gluteus maximus muscle sliding over the greater trochanter when the hip is moved through flexion and extension range of motion (10). Repetitive snapping over the greater trochanter can lead to greater trochanteric bursitis and pain (11). Internal snapping hip syndrome is caused by the iliopsoas tendon gliding over structures in the pelvis. The iliopectineal eminence and femoral head are the most common locations where the iliopsoas can snap. Other reported areas are lesser trochanter exostoses and iliopsoas bursa (12). The intra-articular type are caused by lesions within the hip joint—this commonly includes osteochondral lesions, acetabular labral tears, or loose bodies (13,14). There is typically clicking or catching mechanical symptoms associated with intra-articular pathology.
History and physical exam
Patients typically present in their 2nd or 3rd decade of life and are commonly dancers and athletes (15). Patients will complain of snapping or even feeling of hip dislocation with coxa saltans externa. The patient will also point over the greater trochanter when asked to isolate the site of snapping. Extra-articular variants may have a subacute traumatic event leading to pain. For the intra-articular variant, patients will typically endorse a traumatic event leading to acute pain. They will complain of sensations of clicking and catching more commonly than snapping seen with the extra-articular variant. Patients with intra-articular pathology will localize pain to the anterior groin region.
On physical exam, full range of motion should be assessed with the patient supine in order to identify intra-articular pathology, with comparison to the contralateral side. Dynamic testing for coxa saltans interna can be performed with the patient supine and moving the hip from flexion, adduction, internal rotation to extension, abduction, and external rotation in order to produce snapping of the iliopsoas tendon. Similar testing may be performed for coxa saltans externa, with the patient in the lateral decubitus position with the affected limb facing upwards. The leg may be taken through flexion and extension while palpating the greater trochanter for snapping. The examiner may also place a finger over the iliopsoas or the iliotibial band during the dynamic test to block snapping if thought to be the culprit (10). A positive flexion-adduction-internal rotation impingement test suggests an intra-articular lesion.
Imaging
Diagnosis of coxa saltans externa can generally be made clinically through reproduction of snapping during examination. Ultrasound can also be helpful in detecting real-time tendinous snapping (16). Radiographs and MRI can be useful to evaluate for intra-articular lesions such as loose bodies and labral tears. Evidence of inflammation of the iliopsoas bursa or iliopsoas may be indirect signs of coxa saltans interna. Iliopsoas bursography is the confirmatory test for diagnosis of coxa saltans interna, allowing the provider to visualize snapping under fluoroscopy.
Treatment
Infrequent, asymptomatic snapping does not require aggressive treatment but rather patient education and reassurance. For symptomatic or frequent snapping, conservative management is initiated consisting of rest, NSAIDs, core and hip conditioning program, and avoidance of activities that cause snapping. Formal physical therapy may also be employed, focusing on stretching of involved muscles, activity modification and improving posture (17). Steroid injection may be considered for localized bursitis.
Rarely, patients with coxa saltans externa may not improve following extensive conservative management and surgery is indicated. Several surgical options have been described that focus on lengthening the IT band. Typically a Z-plasty of the IT band is performed with excision of the trochanteric bursa. The surgical literature is limited to small case series. Brignall et al. reported IT band Z-plasty with excellent results though 2 patients complained of persistent dull aching over the greater trochanter and one patient required a reoperation for more extensive Z-plasty. Provencher et al. reported IT band Z-plasty on 8 patients with an average follow up of 22.9 months. All 8 patients had resolution of snapping. One had persistent groin pain but no residual snapping (18-20).
Coxa saltans interna also normally resolves with conservative management. Surgical management consists of lengthening of the iliopsoas tendon. Jacobson et al. lengthened 20 iliopsoas tendons through the tendinous portion of the iliopsoas with a follow up of 25 months. Of the 20 hips, 14 had no snapping postoperatively. Six patients had recurrent snapping but was less frequent and painful compared to preoperative levels. Two hips required reoperation, and three complained of subjective weakness (21). Dobbs et al. described lengthening 11 iliopsoas tendons at the musculotendinous junction through a modified iliofemoral approach with a follow up of approximately 4 years. All patients were able to return to preoperative level without weakness. One patient had recurrent snapping but less frequently and less painful. Two patients had transient decreased sensation in the anterolateral aspect of the thigh (17).
Treatment of the intra-articular type requires addressing the intra-articular pathology such as a labral tear, osteochondral lesion, or loose body. This can be addressed either with hip arthroscopy or an open approach (13).
Pediatric labral tear and femoroacetabular impingement
Epidemiology
In recent years, improvements in hip MRI imaging and hip arthroscopy techniques have grown at a tremendous rate, especially in the pediatric population. Along with this increase has occurred a concomitant increase in the diagnosis and treatment of labral tears in young athletes. Stracciolini et al. looked at a sample of patients presenting to their sports medicine clinic over a 10-year period with a hip injury and found that 23.1% of males and 59% of females presented with labral tears, the most common diagnosis for either subset (22). The acetabular labrum, similar to the glenoid labrum, acts to increase the surface area and stabilize the hip joint; however it also functions similarly to the meniscus acting as a shock absorber providing pressure distribution to protect the articular cartilage.
Labral tears can occur via either acute traumatic or chronic repetitive stresses, presenting with unique symptoms depending on the etiology. Young athletes are especially at risk for acute injuries during sport as a result of planting or cutting movements. It is important to recognize and diagnose the injuries early as there is an association between labral injury and the early onset of osteoarthritis (23). In the setting of cam or pincer lesions of femoroacetabular impingement (FAI), early signs of degenerative labral change can be seen in young adults, especially those with a cam- or combined-type lesion. This is especially true in athletes performing at high levels with increased forces placed upon the joint (24). Other bony disorders including acetabular dysplasia, Legg-Calves-Perthes, SCFE, and coxa valga can also place the labrum at greater risk of injury (25).
History and physical exam
Following an acute injury, athletes will present with sharp groin pain and frequently have mechanical symptoms such as catching and locking. Chronic tears tend to present with an aching type pain exacerbated by repetitive motion, especially flexion.
Physical examination should consist of range of motion testing along with specific tests for impingement and labral pathology. Log roll, FABER, FADIR, and Stinchfield’s test can all illicit pain in patients with labral tears, but cannot exclude many other potential etiologies (26). Extra-articular etiologies of hip pain should be ruled out. Radiographs are useful in evaluating the youth hip for evidence of dysplasia. X-rays with evidence of dysplasia or femoroacetabular impingement (abnormal alpha angle, center-edge angle, Tönnis angle, retroversion, etc.) should raise one’s clinical suspicion of a chronic labral degeneration. Wenger et al found in a study of 31 patients with acetabular labral tears, 87% of patients had at least one radiographic abnormality, while 35% had more than one finding.
Imaging
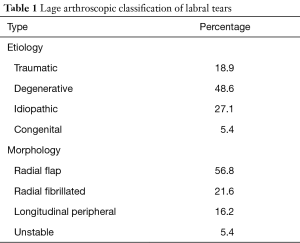
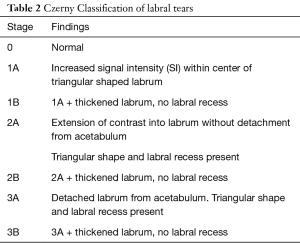
The gold standard for diagnosis of labral tears is magnetic resonance arthrography (MRA), demonstrating a reported sensitivity between 76% and 91% (27). The addition of intra-articular contrast is essential as the sensitivity of standard MR imaging drops to only 30% without arthrography. The initial classification system of labral tears was developed by Lage using arthroscopy, describing the etiology and morphology of tears (Table 1). Czerny developed a classification system of labral tears based on MRA findings with excellent correlation of arthroscopic findings (Table 2). In 2007, Blankenbaker in a retrospective study of patients used MRA correlated with arthroscopic findings to create a system to localize labral tears. The majority of tears were found to be in the anterior-superior aspect of the acetabulum, however tears could be found in all quadrants (28). Localization of the lesion pre-operatively can help guide surgical planning and portal placement. For patients with plain films or MR evidence of FAI pathology, preoperative workup should include a CT scan with 3D reconstructions to properly assess the location and size of associated bony impingement lesions.
Full table
Full table
Treatment
Treatment of acetabular labral lesions frequently starts with trial of non-operative management consisting of rest, NSAIDs, core and hip strengthening, and activity modification. As with most cartilage in the body, biologic repair is minimal or absent as cartilage tends to be an avascular structure (29). In a low demand patient, non-operative management is a reasonable course as pain and symptoms are correlated with activity level. However, young athletes frequently fail conservative management given their activity demands. In patients with early degenerative change or those suspected of having a labral tear, injections can be both diagnostic and therapeutic. For some patients, acute labral tears are painful only in the short-term, and once the initial inflammation subsides, they can remain asymptomatic indefinitely. The presence of FAI pathology in the setting of a labral tear, particularly in the elite athlete, typically will warrant FAI surgery.
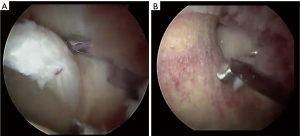
Hip arthroscopy has rapidly become an effective treatment strategy for labral pathology and has been shown to be safe and effective in adolescents (3,23,30,31). It is important to address both the labral tear (Figure 2A) as well as any underlying bony impingement lesions (Figure 2B) at time of hip arthroscopy. Intraoperative fluoroscopy is utilized to ensure no residual deformity.
Contraindications to arthroscopic management of labral tears with underlying FAI include posterior extension of impingement lesions that are difficult to reach, acetabular dysplasia, acetabular retroversion with posterior wall deficiency, excessive femoral retroversion, and osteoarthritis.
Philippon reported a series of 60 adolescents who underwent either arthroscopic debridement or repair of labral tear with a minimum of 2-year follow-up. Patients demonstrated an increased in the modified Harris Hip score from 61 to 90 with no significant difference noted between debridement vs. repair (30). Espinosa et al reported a series of 60 hips that had undergone surgical hip dislocation. At 2-year follow-up, the labral repair group had superior clinical results and radiographic outcomes compared with the resection cohort (32). Larson reported on 94 adolescent patients with a minimum of 3.5-year follow-up and found a 92% improvement in the labral repair group vs. a 68% improvement with debridement (33). Furthermore, high level athletes including professional level have shown excellent return to play rates over 90% after FAI surgery (34,35).
SCFE in young athletes
Epidemiology
SCFE is one of the most common hip conditions affecting adolescents, with an incidence of SCFE of 10.8 per 100,000 children (36). It is characterized by a posterior displacement of the epiphysis through the hypertrophic zone with the metaphysis assuming an anterior and superior position. The injury is a Salter-Harris type 1 physeal fracture, which occurs when a shearing force in excess of the strength of the growth is applied to the femoral head. The average age of presentation is 12.2 years overall, with girls and boys averaging 11.2 and 12.7 years respectively. This is consistent with hypothesis that changes to the physis during the pubertal growth spurt may weaken its integrity (37). Obesity is a well-known risk factor and as the incidence of obesity in children has risen, so too has the incidence of SCFE (36,38).
History and physical exam
Patients with SCFE can present along a spectrum of symptomatology ranging from chronic, dull, aching knee pain to acute, severe hip pain. Typically, patients with an acute slip will present shortened and externally rotated with a decreased ability to internally rotate, flex, and abduct the leg. However, physical exam findings may be subtle, highlighting the importance of clinical suspicion. More commonly, a young athlete who presents with SCFE will not fit the traditional profile. These atypical cases include children less than 10 years old, greater than 16 years old, and/or weight less than the 50th percentile for their age and height, comprising approximately 15% of cases. In these children, it is imperative to search for an underlying cause of physeal weakness. Common etiologies include endocrine disorders (hypothyroid, growth hormone deficiency), renal disease, genetic disorders (Down syndrome, Rubinstein-Taybi disease), and previous radiation therapy (39). One should also be aware that approximately 5% of SCFE are a valgus variant in which the epiphysis is displaced superolaterally, thereby lengthening and limiting adduction of the leg (40). Forty-three percent of patients with this valgus variant presents with an atypical profile.
There are three classification systems upon which SCFEs can be assessed: stability, chronicity, and severity. The simplest, and most commonly discussed is stability. A patient is considered to have a stable SCFE if they are able to weight bear on the affected limb whereas a SCFE is considered unstable if a patient is unable to weight bear, even with the use of assistive devices (crutches, rolling walker, etc.). This classification has gained popularity recently due to its prognostic value as unstable patients are at a higher risk for developing avascular necrosis of the femoral head (41).
Another method of classifying SCFE is based on the chronicity of symptoms ranging from acute, acute-on-chronic, to chronic (Table 3) (42). Finally, SCFE can be graded based on the level of displacement of the epiphysis (Table 4). The Southwick angle is a measure of posterior angulation of the femoral head compared to the neck. This is the angle is measured on the frog lateral view. The angle is measured based on a line drawn down the femoral shaft in comparison to a line perpendicular to the femoral epiphysis. This angle is measured on both the involved and uninvolved hip and the difference of the two angles is calculated to determine slip severity. In the event of bilateral involvement, 12 degrees may be used as the normal angle for comparison (43).
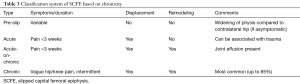
Full table
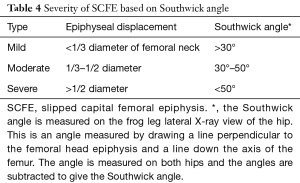
Full table
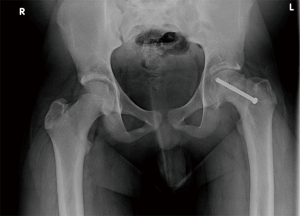
Imaging
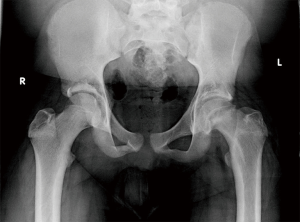
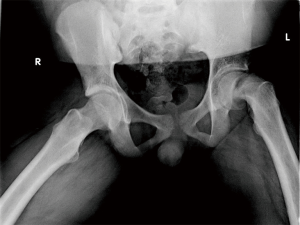
While clinical suspicion for SCFE may be high, ultimately the diagnosis is radiographic. On the AP radiograph, Klein’s line is drawn along the superior femoral neck proximally through the epiphysis; as patients with SCFE suffer a posteromedial displacement of the epiphysis, Klein’s line will no longer intersect the femoral head (Figures 3,4). In a valgus SCFE, one will observe a larger percentage of the femoral head lateral to the Klein’s line. There is no consensus on whether a cross-table or frog-leg is the preferred lateral study. Proponents of the cross-table argue there are less forces across the physis to prevent further displacement in unstable slips. However, the frog-leg is more sensitive in the detection of SCFE and provides better visualization in obese patients (43). As discussed above, the Southwick angle is measured on the frog-leg view and can aid in the assessment of severity.
MR imaging is useful for patients with both minor and severe injuries. With subtle or pre-slip patients, one can visualize widening of the physis, marrow edema of the metaphysis, and/or joint effusion. In severe cases, MR can provide detailed anatomy of the deformity, especially if multi-view radiographs cannot be tolerated. Post-operatively, evaluation of femoral head circulation can be assessed to identify children at risk for avascular necrosis. Computerized tomography, bone scintigraphy, and ultrasound can also be used in the work-up of SCFE, but are not routinely used.
Treatment
Any young athlete presenting with suspected SCFE should be immediately made non-weight bearing until the diagnosis can be confirmed or excluded as avoiding further slip progression is crucial for improved outcomes. Missed or prolonged diagnosis cases can lead to long-term debilitating consequences including avascular necrosis, chondrolysis, cam-type femoral acetabular impingement, and osteoarthritis, requiring reconstruction via osteotomy or arthroplasty.
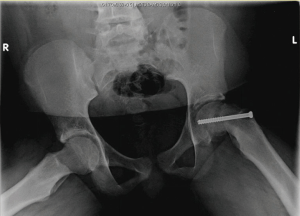
Surgical fixation with a single cannulated screw through the center of the epiphysis provides stabilization until closure of the growth plate occurs and has long been the treatment of choice (Figures 5,6) (44,45). Controversy exists regarding whether closed reduction should occur in the setting of acute slips as evidence suggests that doing so increases the risk of AVN (46,47). This decision is understandably more complicated in high-level young athletes for whom hip dysfunction could be career ending. Fortunately, studies have demonstrated that remodeling with improved range of motion can be expected with in situ pinning (48).
SCFE is bilateral in approximately twenty percent of cases at presentation with thirty to sixty percent of unilateral slips progressing to bilateral involvement, commonly within the first 18 months (49,50). At a minimum close follow-up is required, but some advocate for prophylactic pinning of the uninjured hip. Those in favor of prophylactic pinning advocate that second slips often are unstable with increased risk of osteonecrosis and osteoarthritis. In a study by Hägglund et al., no osteoarthritis was observed in hips which were stabilized prophylactically versus 25% in the monitored group (50). Popejoy et al. suggest that the modified Oxford bone age score may be an effective predictor of contralateral slips to guide management and avoid unnecessary surgery (51).
Post-operative management includes a period of protected weight-bearing with crutches for six-to-eight weeks. Physical therapy begins shortly after surgery, beginning with passive ROM exercises and progressing to full-weight bearing and resistance exercises. Patients may return to sport once they regain full strength and pain-free, typically after 3 to 6 months. Radiographic follow-up should continue until the physis closes. The contralateral hip should be closely monitored for signs of a slip. Hardware removal is generally unnecessary.
Acknowledgments
Funding: None.
Footnote
Provenance and Peer Review: This article was commissioned by the Guest Editors (Alexis Chiang Colvin and Diana Patterson) for the series “Orthopaedic Sports Injuries in Youth” published in Annals of Joint. The article has undergone external peer review.
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/aoj.2018.04.02). The series “Orthopaedic Sports Injuries in Youth” was commissioned by the editorial office without any funding or sponsorship. The authors have no other conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Hawkins D, Metheny J. Overuse injuries in youth sports: biomechanical considerations. Med Sci Sports Exerc 2001;33:1701-7. [Crossref] [PubMed]
- Adirim TA, Cheng TL. Overview of injuries in the young athlete. Sports Med 2003;33:75-81. [Crossref] [PubMed]
- Kocher MS, Kim YJ, Millis MB, et al. Hip arthroscopy in children and adolescents. J Pediatr Orthop 2005;25:680-6. [Crossref] [PubMed]
- Salter RB, Harris WR. Injuries Involving the Epiphyseal Plate. JBJS Am 1963;45:587. [Crossref]
- Metzmaker JN, Pappas AM. Avulsion fractures of the pelvis. Am J Sports Med 1985;13:349-58. [Crossref] [PubMed]
- Rossi F, Dragoni S. Acute avulsion fractures of the pelvis in adolescent competitive athletes: prevalence, location and sports distribution of 203 cases collected. Skeletal Radiol 2001;30:127-31. [Crossref] [PubMed]
- Schuett DJ, Bomar JD, Pennock AT. J Pediatr Orthop 2015;35:617-23. [Crossref] [PubMed]
- Lazović D, Wegner U, Peters G, et al. Ultrasound for diagnosis of apophyseal injuries. Knee Surg Sports Traumatol Arthrosc 1996;3:234-7. [Crossref] [PubMed]
- McKinney BI, Nelson C, Carrion W. Apophyseal avulsion fractures of the hip and pelvis. Orthopedics 2009;32:42. [Crossref] [PubMed]
- Allen WC, Cope R. Coxa Saltans: The Snapping Hip Revisited. J Am Acad Orthop Surg 1995;3:303-8. [Crossref] [PubMed]
- Zoltan DJ, Clancy WG, Keene JS. A new operative approach to snapping hip and refractory trochanteric bursitis in athletes. Am J Sports Med 1986;14:201-4. [Crossref] [PubMed]
- Schaberg JE, Harper MC, Allen WC. The snapping hip syndrome. Am J Sports Med 1984;12:361-5. [Crossref] [PubMed]
- Ikeda T, Awaya G, Suzuki S, et al. Torn acetabular labrum in young patients. Arthroscopic diagnosis and management. J Bone Joint Surg Br 1988;70:13-6. [Crossref] [PubMed]
- Yen YM, Lewis CL, Kim YJ. Understanding and Treating the Snapping Hip. Sports Med Arthrosc Rev 2015;23:194-9. [Crossref] [PubMed]
- Howse AJ. Orthopaedists aid ballet. Clin Orthop 1972;52-63. [PubMed]
- Choi YS, Lee SM, Song BY, et al. Dynamic sonography of external snapping hip syndrome. J Ultrasound Med 2002;21:753-8. [Crossref] [PubMed]
- Dobbs MB, Gordon JE, Luhmann SJ, et al. Surgical correction of the snapping iliopsoas tendon in adolescents. J Bone Joint Surg Am 2002;84-A:420-4. [Crossref] [PubMed]
- Provencher MT, Hofmeister EP, Muldoon MP. The surgical treatment of external coxa saltans (the snapping hip) by Z-plasty of the iliotibial band. Am J Sports Med 2004;32:470-6. [Crossref] [PubMed]
- Brignall CG, Stainsby GD. The snapping hip. Treatment by Z-plasty. J Bone Joint Surg Br 1991;73:253-4. [Crossref] [PubMed]
- Larsen E, Johansen J. Snapping hip. Acta Orthop Scand 1986;57:168-70. [Crossref] [PubMed]
- Jacobson T, Allen WC. Surgical correction of the snapping iliopsoas tendon. Am J Sports Med 1990;18:470-4. [Crossref] [PubMed]
- Stracciolini A, Yen YM, d’Hemecourt PA, et al. Sex and growth effect on pediatric hip injuries presenting to sports medicine clinic. J Pediatr Orthop B 2016;25:315-21. [Crossref] [PubMed]
- Bayley G, Poitras S, Parker G, et al. Hip arthroscopy in patients less than 25 years of age in the treatment of labral tears: aetiology and clinical outcomes. Hip Int 2017;27:436-42. [Crossref] [PubMed]
- Byrd JW. Femoroacetabular impingement in athletes: current concepts. Am J Sports Med 2014;42:737-51. [Crossref] [PubMed]
- Wenger DE, Kendell KR, Miner MR, et al. Acetabular labral tears rarely occur in the absence of bony abnormalities. Clin Orthop Relat Res 2004;145-50. [Crossref] [PubMed]
- Frank JS, Gambacorta PL, Eisner EA. Hip pathology in the adolescent athlete. J Am Acad Orthop Surg 2013;21:665-74. [Crossref] [PubMed]
- Toomayan GA, Holman WR, Major NM, et al. Sensitivity of MR arthrography in the evaluation of acetabular labral tears. AJR Am J Roentgenol 2006;186:449-53. [Crossref] [PubMed]
- Blankenbaker DG, De Smet AA, Keene JS, et al. Classification and localization of acetabular labral tears. Skeletal Radiol 2007;36:391-7. [Crossref] [PubMed]
- Petersen W, Petersen F, Tillmann B. Structure and vascularization of the acetabular labrum with regard to the pathogenesis and healing of labral lesions. Arch Orthop Trauma Surg 2003;123:283-8. [Crossref] [PubMed]
- Philippon MJ, Ejnisman L, Ellis HB, et al. Outcomes 2 to 5 years following hip arthroscopy for femoroacetabular impingement in the patient aged 11 to 16 years. Arthroscopy 2012;28:1255-61. [Crossref] [PubMed]
- Roy DR. Arthroscopy of the hip in children and adolescents. J Child Orthop 2009;3:89-100. [Crossref] [PubMed]
- Espinosa N, Rothenfluh DA, Beck M, et al. Treatment of femoro-acetabular impingement: preliminary results of labral refixation. J Bone Joint Surg Am 2006;88:925-35. [PubMed]
- Larson CM, Giveans MR, Stone RM. Arthroscopic debridement versus refixation of the acetabular labrum associated with femoroacetabular impingement: mean 3.5-year follow-up. Am J Sports Med 2012;40:1015-21. [Crossref] [PubMed]
- Byrd JW, Jones KS. Hip arthroscopy in athletes: 10-year follow-up. Am J Sports Med 2009;37:2140-3. [Crossref] [PubMed]
- Fabricant PD, Heyworth BE, Kelly BT. Hip arthroscopy improves symptoms associated with FAI in selected adolescent athletes. Clin Orthop 2012;470:261-9. [Crossref] [PubMed]
- Lehmann CL, Arons RR, Loder RT, et al. The epidemiology of slipped capital femoral epiphysis: an update. J Pediatr Orthop 2006;26:286-90. [Crossref] [PubMed]
- Kandzierski G, Matuszewski L, Wojcik A. Shape of growth plate of proximal femur in children and its significance in the aetiology of slipped capital femoral epiphysis. Int Orthop 2012;36:2513-20. [Crossref] [PubMed]
- Murray AW, Wilson NI. Changing incidence of slipped capital femoral epiphysis: a relationship with obesity? J Bone Joint Surg Br 2008;90:92-4. [Crossref] [PubMed]
- Whyte N, Sullivan C. Slipped Capital Femoral Epiphysis in Atypical Patients. Pediatr Ann 2016;45:e128-34. [Crossref] [PubMed]
- Loder RT, O’Donnell PW, Didelot WP, et al. Valgus slipped capital femoral epiphysis. J Pediatr Orthop 2006;26:594-600. [Crossref] [PubMed]
- Loder RT, Aronson DD, Greenfield ML. The epidemiology of bilateral slipped capital femoral epiphysis. A study of children in Michigan. J Bone Joint Surg Am 1993;75:1141-7. [Crossref] [PubMed]
- Bittersohl B, Hosalkar HS, Zilkens C, et al. Current concepts in management of slipped capital femoral epiphysis. Hip Int 2015;25:104-14. [Crossref] [PubMed]
- Jarrett DY, Matheney T, Kleinman PK. Imaging SCFE: diagnosis, treatment and complications. Pediatr Radiol 2013;43:S71-82. [Crossref] [PubMed]
- Loder RT, Richards BS, Shapiro PS, et al. Acute slipped capital femoral epiphysis: the importance of physeal stability. J Bone Joint Surg Am 1993;75:1134-40. [Crossref] [PubMed]
- Wensaas A, Svenningsen S, Terjesen T. Long-term outcome of slipped capital femoral epiphysis: a 38-year follow-up of 66 patients. J Child Orthop 2011;5:75-82. [Crossref] [PubMed]
- Uglow MG, Clarke NM. The management of slipped capital femoral epiphysis. J Bone Joint Surg Br 2004;86:631-5. [Crossref] [PubMed]
- Kitano T, Nakagawa K, Wada M, et al. Closed reduction of slipped capital femoral epiphysis: high-risk factor for avascular necrosis. J Pediatr Orthop B 2015;24:281-5. [Crossref] [PubMed]
- Hansson G, Billing L, Hogstedt B, et al. Long-term results after nailing in situ of slipped upper femoral epiphysis. A 30-year follow-up of 59 hips. J Bone Joint Surg Br 1998;80:70-7. [Crossref] [PubMed]
- Riad J, Bajelidze G, Gabos PG. Bilateral slipped capital femoral epiphysis: predictive factors for contralateral slip. J Pediatr Orthop 2007;27:411-4. [Crossref] [PubMed]
- Hägglund G. Pinning the slipped and contralateral hips in the treatment of slipped capital femoral epiphysis. J Child Orthop 2017;11:110-3. [Crossref] [PubMed]
- Popejoy D, Emara K, Birch J. Prediction of contralateral slipped capital femoral epiphysis using the modified Oxford bone age score. J Pediatr Orthop 2012;32:290-4. [Crossref] [PubMed]
Cite this article as: Chang AL, Cirino C, Anthony SG. Orthopaedic sports injuries in youth: the hip. Ann Joint 2018;3:36.