
Elbow injuries in the pediatric athlete
Introduction
As youth sports participation continues to expand, the incidence of sport-related elbow injuries has surged amongst the pediatric population. The majority of sport-related pathology falls into the category of ‘overuse’ injuries, and occurs more often in overhead sports, such as baseball, softball, and tennis, or those sports that require repetitive loading of the elbow joint such as gymnastics and weightlifting. The increased incidence of overuse injuries of the elbow has closely paralleled the trend towards sports specialization at a young age, with adolescent athletes concentrating on a single sport year-round (1). Acute, traumatic elbow injuries are less common in youth sports.
The primary etiology of pediatric sport-related elbow injuries is repetitive stress to the skeletally immature elbow. An understanding of elbow development and sport-specific kinematics is essential to proper diagnosis and treatment of sport-related elbow injuries. This review will discuss the developmental anatomy of the pediatric elbow as it pertains to sport-related injuries. It will focus in detail on the diagnosis and treatment of the most common injuries encountered in pediatric athletes including medial elbow valgus overload injuries [medial epicondyle apophysitis, medial epicondyle avulsion fractures, and ulnar collateral ligament (UCL) injuries], olecranon apophysitis and stress fractures, and osteochondral injuries of the capitellum. It will end with a discussion regarding current options for prevention of overuse injuries in adolescent athletes.
Anatomy and throwing mechanics
The pediatric elbow contains six ossification centers of endochondral bone formation. These centers ossify in a reliable pattern, although timing can vary based on patient sex and ethnicity (2,3). The capitellum normally appears by age 1 years, followed by the radial head, medial epicondyle, trochlea, olecranon, and lateral epicondyle at 2-year increments. The centers slowly progress to maturity and fusion, with the medial epicondyle fusing last between 14–16 years of age (2,4).
The pediatric elbow shares the same soft tissue and osseous static and dynamic stabilizers as the mature joint, with the addition, however, of developing physes and apophyses. The physes are the weakest portion of the ligamentous and musculotendinous unit attachments, altering force distribution and creating distinct pathologies (5-7). While adults may injure stabilizing ligaments in acute or attritional fashion, the pediatric athlete will more likely be affected at the level of the physes prior to fusion (5,6).
Throwing athletes place unique stress on the developing elbow. The overhead throw requires kinetic chain activation starting with lower extremity stride, followed by coordinated motion through the pelvis, trunk and upper extremity. The sequence of arm movements is further separated into six phases of throwing (8). The late cocking and acceleration phases, during which extreme valgus force is placed upon the elbow, are of importance to joint pathology (8,9). Medial sided structures such as the flexor-pronator mass, medial epicondyle, and UCL produce high levels of varus torque to counter the external forces, and are at risk for injury. Conversely, the lateral elbow column, particularly the radiocapitellar joint, faces considerable compressive loads and is also prone to attritional injury (8).
Medial sided elbow injuries
Medial sided elbow injuries in skeletally immature athletes have increased in incidence with the increasing sports participation and single sport specialization (1,10). Most commonly associated with throwing sports such as baseball and softball, medial sided elbow pathology is due to repetitive valgus stress on the medial stabilizers of the elbow. Medial sided elbow injuries fit under the umbrella term of ‘valgus overload injuries’ with the specific pathology dependent on the skeletal maturity of the athlete. The skeletally immature athlete with an unfused medial apophysis is at risk of medial apophysitis, more commonly known as “Little Leaguer’s elbow”. This is due to the fact that the developing apophysis and surrounding epiphyseal plate is structurally weaker than the surrounding tissues. As the athlete moves towards apophyseal fusion he or she is at risk for apophyseal separation and apophyseal avulsion fractures, while the skeletally mature adolescent athlete is at risk for injuries to the UCL consistent with similar injuries in the adult population.
A number of risk factors have been identified for development of medial sided elbow injuries and valgus overload syndrome. These include poor sport specific biomechanics, relative core and lower extremity weakness, and increased pitch count and type of pitch thrown (9,11,12). Treatment is dependent on the age and skeletal maturity of the patient as well as the patient’s future goals for sports participation.
Medial epicondyle apophysitis (little leaguer’s elbow)
Medial epicondyle apophysitis, also known as Little Leaguer’s elbow, is defined as inflammation of the apophysis of the medial epicondyle leading to pain and discomfort with sport-related activities. It occurs due to repetitive stress and traction at the origin of the flexor-pronator mass on the developing medial epicondyle. It is seen almost exclusively in overhead throwing athletes and occurs during the late cocking phase of throwing when maximum physiologic valgus stress is placed on the medial elbow structures. This leads to a repetitive traction injury to the medial epicondyle, which can cause widening of the apophysis and inflammation to the medial elbow.
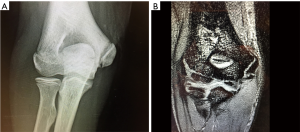
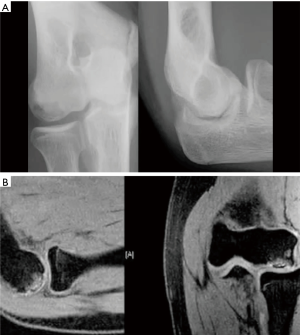
Patients at risk for medial epicondyle apophysitis are younger, generally under the age of 10, with open physes (13). As the developing apophysis is weaker than the surrounding soft tissue stabilizers of the medial elbow, it is at highest risk for injury with repetitive valgus stress. Patients will report pain and discomfort to the medial epicondyle with throwing and may report decreased velocity, however valgus instability is rare (14). Physical examination can reveal swelling to the medial elbow with tenderness to palpation directly over the medial epicondyle. While the diagnosis is ultimately clinical, radiographs can assist with diagnosis and may show widening of the medial apophysis compared to the contralateral unaffected side or fragmentation to the medial apophysis (15). Magnetic resonance imaging, while not required for diagnosis, will demonstrate varying levels of inflammation and widening of the medial apophysis (16) (Figure 1).
Treatment is conservative and there is little to no role for operative intervention. Patients should be advised to cease all throwing activity and begin a physical therapy regimen focusing on core and lower extremity strengthening (17). This is grounded in the notion that young overhead athletes with elbow injuries do not appropriately utilize their core and lower extremities to generate velocity during the throwing motion, leading to increased stress on the medial elbow (9). Gradual return to throwing should be initiated at 6 weeks when there is no longer tenderness to palpation over the medial elbow. Return to play is allowed when the patient can participate in normal sport-related activities without evidence of pain or discomfort.
Medial epicondyle fractures
Medial epicondyle fractures represent 10–20% of all pediatric elbow fractures (18). These can occur either with direct trauma to the elbow (with or without an associated elbow dislocation) or due to an acute avulsion from valgus overload during overhead activity, the latter occurring in patients at or near the time of apophyseal fusion. Regardless of mechanism of injury, immobilization and nonoperative management of medial epicondyle fractures has demonstrated excellent results with low rates of complication and high rates of return to normal elbow function and activity (19,20). Operative intervention has been advocated only in those instances of significant medial epicondyle displacement, the presence of incarcerated fragments within the ulnohumeral joint, or ulnar nerve entrapment and has demonstrated excellent outcomes with return to normal elbow function (18,21,22).
Treatment of medial epicondyle fractures in the overhead athlete presents a unique situation requiring careful consideration. While malunion of a displaced medial epicondyle fracture may not affect the general population, it could lead to valgus laxity or alter throwing biomechanics in the overhead athlete. This has led some to advocate for more aggressive operative intervention in treating displaced medial epicondyle fractures in the throwing athlete.
Lawrence and colleagues retrospectively reviewed 20 athletes who sustained acute medial epicondyle fractures, 6 of which were treated nonoperatively with immobilization and 14 of which underwent open reduction and internal fixation (23). Nonoperative management consisted of 3–4 weeks of long arm cast immobilization in 70°–90° of elbow flexion with the forearm in neutral rotation. This was followed by conversion to a removable posterior splint with gentle guided range of motion and then to physical therapy 6–8 weeks after injury. Operative management was indicated for greater than 5–8 mm of medial epicondyle displacement or the presence of valgus elbow laxity on exam. Treatment involved a direct medial approach with open reduction and internal fixation with a cannulated screw. This was followed by a similar period of immobilization and return to function as in nonoperative management. They reported that all 20 patients were able to return to sport at the appropriate level. Subgroup analysis of 14 overhead athletes, 6 treated nonoperatively and 8 treated operatively, revealed equally good outcomes and rate of return to play.
Osbahr and colleagues similarly reviewed 8 youth baseball players with an average age of 13 who sustained acute medial epicondyle avulsion fractures while throwing with an average fracture displacement of 5.1 mm (24). Patients with greater than 5mm of displacement (n=3) were indicated for open reduction and internal fixation while those with less than 5 mm of displacement (n=5) were treated nonoperatively with immobilization. All patients had excellent results with return to play approximately 7 months after the initial injury.
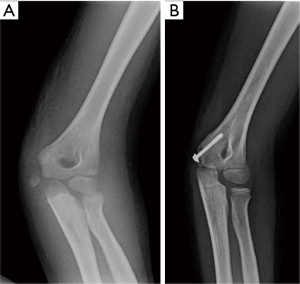
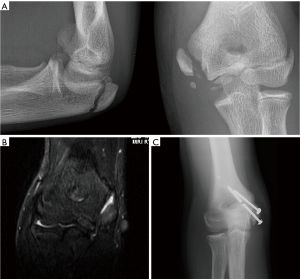
These results suggest that excellent outcomes and return to play can be expected with appropriate management of medial epicondyle fractures in overhead athletes. While there is no specific amount of displacement that should prompt operative intervention, the presence of valgus instability on examination or greater than 5 mm of radiographic displacement can be considered acceptable indications for open reduction and internal fixation with use of one or two cannulated screws (Figures 2,3).
UCL injuries
Injuries to the anterior band of UCL occur after ossification and fusion of the medial epicondyle. Repetitive valgus stress of the UCL with overhead activity can lead to partial tearing or rupture of the UCL. While the incidence UCL injury continues to increase in pediatric athletes, this is considered an injury of skeletal maturity and is treated similar to UCL injuries in adult athletes.
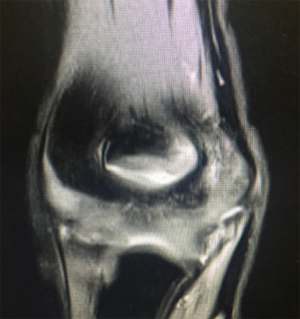
Patients with UCL pathology will report pain over the medial elbow with overhead activity and decreased sport-specific performance. Diagnosis is based on patient history, clinical examination, and radiographic findings. The most useful examination maneuver is the ‘moving valgus stress test’ whereby the elbow is flexed to 90° and the forearm is supinated. A valgus stress is then created and the elbow is taken through a full flexion-extension arc of motion. Pain or subjective apprehension between 70° and 120° of elbow flexion is highly specific for UCL pathology (25). Valgus stress radiographs can demonstrate medial gapping of the ulnohumeral joint and ultrasound is useful in diagnosis of partial tears. However, MRI is the diagnostic imaging modality of choice for evaluating the UCL (26-28) (Figure 4).
Treatment of UCL injuries in the throwing athlete should be patient-specific and based on both the presenting pathology and the future athletic goals of the patient. Care must be taken to fully explain treatment options and postoperative expectations as considerable public misconceptions continue to exist regarding outcomes after UCL reconstruction, especially the perception that UCL reconstruction can help an athlete improve their performance (29,30).
Treatment options for UCL ruptures in pediatric patients are dependent both the location of the injury as well as surgeon preference. There has been little success treating full thickness UCL injuries nonoperatively. Rettig and colleagues retrospectively evaluated 31 throwing athletes with UCL ruptures treated nonoperatively and reported a 42% rate of return to play, however they were unable to identify any specific predictive measure suggesting who would benefit from nonoperative management (31).
A number of operative techniques have been described for reconstruction of the UCL. These include the modified Jobe technique, the docking technique, and hybrid fixation techniques (28). The technical operative considerations of UCL reconstruction are beyond the scope of this review. However, looking specifically at adolescent athletes, UCL reconstruction provides reliable results with high rates of return to sport at or above baseline level consistent with results demonstrated in the adult population (32,33).
An injury pattern unique to younger athletes is the avulsion of the UCL either from the origin at the medial epicondyle or at the insertion at the sublime tubercle (34-36). Savoie and colleagues reviewed the results of primary repair of proximal or distal UCL injuries to avoid the need for ligament reconstruction. They reported that, in those instances where the injury was either very proximal or distal along the length of the ligament, patients did well with primary repair, with 93% of athletes (56/60) returning to play within 6 months of surgery (37). This suggests that there are specific instances where primary repair is appropriate thus avoiding the morbidity and prolonged rehabilitation associated with autograft reconstruction.
There has been recent interest in the treatment of partial UCL tears, especially with regards the utility of biologic adjuvants to improve healing. Previously, treatment of partial UCL tears had included cessation of overhead activity followed by gradual return to sport, with surgical intervention reserved for those that have failed an initial course of nonoperative management. Podesta and colleagues evaluated the utility of a series of platelet-rich-plasma (PRP) injections to improve and accelerate healing of partial UCL tears (38). They reported that PRP injections in conjunction with an initial period of rest followed by gradual resumption of throwing activities provided high rates of return to play, with 30 of 34 patients returning to baseline level of sport. While these results are promising, there is still no consensus of the role of PRP in the treatment of UCL injuries (39).
Olecranon apophysitis and stress fractures
Injury to the olecranon in pediatric athletes is due repetitive elbow extension and the subsequent stress of triceps contraction on the developing olecranon (40,41). This injury pattern is most commonly seen in repetitive overhead athletes involved in sports that load the elbow in flexion such as gymnastics and overhead throwing athletes. Repetitive traction on the olecranon by the contracting triceps can lead to injuries similar to those previously described to the medial epicondyle.
The type of injury sustained is dependent on the stage of maturation of the olecranon apophysis. Prior to apophyseal fusion, patients will present with a traction apophysitis. They will report pain with activities requiring resisted elbow extension. Physical examination will demonstrate tenderness over the olecranon and pain with resisted elbow extension from a flexed position (13). Radiographs may demonstrate widening of the olecranon apophysis compared to the contralateral unaffected side and sclerosis of the apophysis (42). During or after fusion of the olecranon apophysis, patients are at risk for developing stress reactions and stress fractures to the olecranon. While the clinical examination is similar to a traction apophysitis, radiographic findings may be subtle or non-existent. MRI or CT evaluation can assist in diagnosis of olecranon stress reaction or fractures (43).
Treatment for both olecranon apophysitis and stress fractures consists of cessation of activity, a brief period of immobilization, gradual guided return to motion, followed by return to play 3–6 months after initiation of treatment. Those patients that fail nonoperative management may require open reduction and internal fixation with tension band construct, cannulated screws, or a combination of the two. Excellent results with high rates of return to play have been reported after surgical management for olecranon stress fractures that had failed nonoperative management in adolescent and young adult athletes (44,45).
Osteochondral lesions of the capitellum
Valgus force produced through the throwing motion applies compressive loads to the radiocapitellar joint. Gymnasts are similarly affected, axially loading the entire articular surface through upper extremity weight bearing maneuvers (46) (Figure 5). These repetitive loads place athletes at risk for damage to the osteochondral structures of the lateral elbow, with the developing capitellum particularly susceptible (47).

Capitellar lesions present with insidious onset lateral elbow pain during activity, increasing stiffness, and inability to perform at previous level of sport. Exam findings include swelling and effusion, point tenderness over the capitellum, and loss of 15°–20° of extension (47,48). The active radiocapitellar compression test can elicit pain when the examiner axially loads the elbow in extension while pronating and supinating the forearm (48,49). Standard AP and lateral projections are primarily utilized, while additional AP views in 45o of flexion can aid in capitellar visualization (50,51).
Osteochondral lesions of the capitellum in pediatric athletes are grouped into two main pathologies. Panner’s disease occurs in younger patients, generally between the ages of 8–12. This period represents an early stage in the ossification process during which the entire ossific nucleus is affected (47,52). Osteochondritis dissecans (OCD) lesions occur in older athletes, generally over the age of 11. As the capitellum nears full ossification, the epiphyseal cartilage thins significantly, placing the weak subchondral bone at risk (47,53,54). The pathogenesis of both diseases is hypothesized to be vascular in nature. The developing capitellar epiphysis maintains a relatively tenuous blood supply, supplied by only 1 or 2 perforating arteries from the posterior aspect of the distal humerus (46,55). Repetitive stress and overuse may compromise these vessels, injuring the ossific nucleus and subchondral bone (49).
In Panner’s disease, plain radiographs can demonstrate involvement of the entire capitellar ossific nucleus, with flattening, sclerosis, and loss of volume (47,53). MRI findings differ upon disease phase, exhibiting low intensity T1 and T2 signal of the lesion during early ischemia, and increasing T2 intensity upon late revascularization (53). Full recovery is expected with conservative management involving cessation of sport-related activities and non-steroidal anti-inflammatory medications (47,54). Repeat radiographs after treatment will show reconstitution of the capitellum over time although residual deformity may remain (47,52,53).
OCD can present in varying degrees of severity, and are more often associated with overhead throwing athletes (47,53). In addition to pain and stiffness, patients may report symptoms of grinding and locking. Crepitus on examination raises the suspicion for unstable lesions or loose bodies (47). Radiographs show focal fragmentation, flattening at the articular surface, cortical irregularities, and subchondral lucency (53). MRI may demonstrate edema of the subchondral bone indicating a pre-collapse state (Figure 6). This modality is also useful in evaluating the integrity of the articular surface, and may show signs of an unstable injury such cartilage tears, displaced osteochondral fragments, and loose bodies within the joint (2).
Multiple classification systems have been described for OCD as prognostic aids and treatment guides. Current grading schemes take into account lesion chronicity, radiographic signs, and arthroscopic findings (47,49,53,56). The key determinant in dictating treatment is whether the osteochondral lesion is stable or unstable. In stable lesions, the articular cartilage layer and subchondral stability is maintained. Initial treatment is conservative, including cessation of throwing activities with or without a period of hinged elbow bracing followed by a physical therapy and return to throwing in 3 to 6 months (50,56,57). These methods have shown reliable recovery for stable OCD lesions with radiographic evidence of healing in 83% to 93% and 78% to 88% return to previous level of play (42,57).
Unstable osteochondral lesions are defined as those associated with collapsed subchondral bone, displaced osteochondral fragments, and loose bodies. Multiple treatment options have been described for unstable osteochondral lesions and those lesions that have failed conservative management. These include reduction and fixation of the chondral fragment, lesion debridement, subchondral drilling, and abrasion chondroplasty. The specific treatment utilized is dependent on patient age, future athletic goals, and the size and thickness of the fragment.
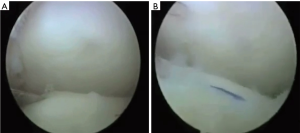
Stable lesions that have failed nonoperative measures are generally treated with subchondral drilling (58). Small unstable osteochondral lesions or cartilage shear fractures can be excised, while attempts should be made to fix large free-floating osteochondral fragments (56) (Figure 7). Although outcomes scores and pain improve after surgery, many authors report poor rates of return to sport (59-65). Osteochondral grafting and cartilage transplantation are reconstructive options for large defects not amenable to fixation. These techniques have also shown consistent postoperative improvement in pain and function, but variable rates of return to sport (56,66,67).
Injury prevention and rehabilitation
There has been a recent dramatic increase in the number of surgical procedures for pediatric athletes with elbow pathology (1,10,68). A number of factors have been identified as being risk factors for elbow injuries in young athletes. Elevated single game and total season pitch counts, playing the position of pitcher or catcher, poor throwing biomechanics, and pitching while fatigued have all been associated with increased risk for elbow injury (1,9,10,69). Contrary to popular belief, throwing breaking pitches at a young age (curveball, slider) has not been shown to increase risk for elbow injury (11,12).
An understanding of the risk factors for elbow injury has led to a focus on prevention of elbow injuries by limiting the number of throws for young athletes throughout a year. After evaluation of available data on risk factors for elbow injuries in throwing athletes, Fleisig and colleagues published a series of recommendations for injury prevention. These include a focus on proper throwing mechanics and utilization of the core and lower extremities throughout the throwing motion, identifying and addressing in-game fatigue, limiting total game and total season pitches, avoiding pitching on multiple teams in multiple leagues, and complete cessation of throwing for at least 2–3 months per year (1).
Based on these recommendations, Little League Baseball, in conjunction with USA baseball, has advocated for pitch count monitoring to decrease the risk of injury. They suggest daily pitch count limitations in an age-based graduated fashion with associated recommendations for periods of rest between pitching. They also recommend against playing the catcher position after throwing more than 40 pitches in a game (70,71). While a focus on injury prevention and proper pitching biomechanics is important, especially in younger athletes, a decrease in injuries after the institution of pitch count rules and safe pitching campaigns has yet to be borne out in the literature. Concern remains for factors such as year-round play and participation on multiple teams which cannot be easily regulated by a single sporting governance.
Throwing rehabilitation is recommended for prevention of injury, treatment for minor pathology, and during recovery after surgical intervention. While training is tailored to individual needs, most programs follow a similar regimen. Major deficits are first addressed, including core stabilization, leg strengthening, and global flexibility (72,73). This allows for progressive focus on the upper extremity kinetic chain, including scapular stabilizers, rotator cuff, and distal arm musculature (73,74). Finally, players complete a graduated throwing program and return to sport, with the entire process concluding over a 3–12 months period based on severity of initial injury (72,74).
Conclusions
The developing elbow is at risk for overuse injuries in pediatric athletes, especially those that participate in overhead and throwing sports. The type of injury is dependent on the status of elbow apophyseal and physeal maturation and the type of load placed across the elbow. Common injuries include medial epicondyle apophysitis and avulsion fractures, UCL rupture, olecranon apophysitis and stress fractures, Panner’s disease, and OCD of the capitellum. Treatment is dependent on the age and future sport-specific goals of the patient. Many conditions can be treated nonoperatively with sport cessation and physical therapy, however there is a role for surgical management. Regardless of the condition, most athletes are able to return to baseline levels of pre-injury activity. A recent focus on injury prevention has emerged with emphasis on pitch count limits and proper mechanics. Further research is required to better delineate optimal treatment methods, surgical indications, and the role and scope of preventative measures.
Acknowledgments
Funding: None.
Footnote
Provenance and Peer Review: This article was commissioned by the Guest Editors (Alexis Chiang Colvin and Diana Patterson) for the series “Orthopaedic Sports Injuries in Youth” published in Annals of Joint. The article has undergone external peer review.
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/aoj.2018.03.02). The series “Orthopaedic Sports Injuries in Youth” was commissioned by the editorial office without any funding or sponsorship. The authors have no other conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Fleisig GS, Andrews JR. Prevention of elbow injuries in youth baseball pitchers. Sports Health 2012;4:419-24. [Crossref] [PubMed]
- Iyer RS, Thapa MM, Khanna PC, et al. Pediatric bone imaging: imaging elbow trauma in children--a review of acute and chronic injuries. AJR Am J Roentgenol 2012;198:1053-68. [Crossref] [PubMed]
- Cheng JC, Wing-Man K, Shen WY, et al. A new look at the sequential development of elbow-ossification centers in children. J Pediatr Orthop 1998;18:161-7. [Crossref] [PubMed]
- Benjamin HJ, Briner WW Jr. Little league elbow. Clin J Sport Med 2005;15:37-40. [Crossref] [PubMed]
- Ireland ML, Hutchinson MR. Upper extremity injuries in young athletes. Clin Sports Med 1995;14:533-69. [PubMed]
- Hutchinson MR, Ireland ML. Overuse and throwing injuries in the skeletally immature athlete. Instr Course Lect 2003;52:25-36. [PubMed]
- Magra M, Caine D, Maffulli N. A review of epidemiology of paediatric elbow injuries in sports. Sports Med 2007;37:717-35. [Crossref] [PubMed]
- Fleisig GS, Barrentine SW, Escamilla RF, et al. Biomechanics of overhand throwing with implications for injuries. Sports Med 1996;21:421-37. [Crossref] [PubMed]
- Davis JT, Limpisvasti O, Fluhme D, et al. The effect of pitching biomechanics on the upper extremity in youth and adolescent baseball pitchers. Am J Sports Med 2009;37:1484-91. [Crossref] [PubMed]
- Olsen SJ 2nd, Fleisig GS, Dun S, et al. Risk factors for shoulder and elbow injuries in adolescent baseball pitchers. Am J Sports Med 2006;34:905-12. [Crossref] [PubMed]
- Dun S, Loftice J, Fleisig GS, et al. A biomechanical comparison of youth baseball pitches: is the curveball potentially harmful? Am J Sports Med 2008;36:686-92. [Crossref] [PubMed]
- Nissen CW, Westwell M, Ounpuu S, et al. A biomechanical comparison of the fastball and curveball in adolescent baseball pitchers. Am J Sports Med 2009;37:1492-8. [Crossref] [PubMed]
- Makhni EC, Jegede KA, Ahmad CS. Pediatric elbow injuries in athletes. Sports Med Arthrosc 2014;22:e16-24. [Crossref] [PubMed]
- Klingele KE, Kocher MS. Little league elbow: valgus overload injury in the paediatric athlete. Sports Med 2002;32:1005-15. [Crossref] [PubMed]
- Hang DW, Chao CM, Hang YS. A clinical and roentgenographic study of Little League elbow. Am J Sports Med 2004;32:79-84. [Crossref] [PubMed]
- Wei AS, Khana S, Limpisvasti O, et al. Clinical and magnetic resonance imaging findings associated with Little League elbow. J Pediatr Orthop 2010;30:715-9. [Crossref] [PubMed]
- Gregory B, Nyland J. Medial elbow injury in young throwing athletes. Muscles Ligaments Tendons J 2013;3:91-100. [PubMed]
- Gottschalk HP, Eisner E, Hosalkar HS. Medial epicondyle fractures in the pediatric population. J Am Acad Orthop Surg 2012;20:223-32. [Crossref] [PubMed]
- Louahem DM, Bourelle S, Buscayret F, et al. Displaced medial epicondyle fractures of the humerus: surgical treatment and results. A report of 139 cases. Arch Orthop Trauma Surg 2010;130:649-55. [Crossref] [PubMed]
- Knapik DM, Fausett CL, Gilmore A, et al. Outcomes of nonoperative pediatric medial humeral epicondyle fractures with and without associated elbow dislocation. J Pediatr Orthop 2017;37:e224-8. [Crossref] [PubMed]
- Kamath AF, Baldwin K, Horneff J, et al. Operative versus non-operative management of pediatric medial epicondyle fractures: a systematic review. J Child Orthop 2009;3:345-57. [Crossref] [PubMed]
- Farsetti P, Potenza V, Caterini R, et al. Long-term results of treatment of fractures of the medial humeral epicondyle in children. J Bone Joint Surg Am 2001;83-A:1299-305. [Crossref] [PubMed]
- Lawrence JT, Patel NM, Macknin J, et al. Return to competitive sports after medial epicondyle fractures in adolescent athletes: results of operative and nonoperative treatment. Am J Sports Med 2013;41:1152-7. [Crossref] [PubMed]
- Osbahr DC, Chalmers PN, Frank JS, et al. Acute, avulsion fractures of the medial epicondyle while throwing in youth baseball players: a variant of Little League elbow. J Shoulder Elbow Surg 2010;19:951-7. [Crossref] [PubMed]
- O'Driscoll SW, Lawton RL, Smith AM. The "moving valgus stress test" for medial collateral ligament tears of the elbow. Am J Sports Med 2005;33:231-9. [Crossref] [PubMed]
- Zellner B, May MM. Elbow injuries in the young athlete--an orthopedic perspective. Pediatr Radiol 2013;43:S129-34. [Crossref] [PubMed]
- Smith W, Hackel JG, Goitz HT, et al. Utilization of sonography and a stress device in the assessment of partial tears of the ulnar collateral ligament in throwers. Int J Sports Phys Ther 2011;6:45-50. [PubMed]
- Bruce JR, Hess R, Joyner P, et al. How much valgus instability can be expected with ulnar collateral ligament (UCL) injuries? A review of 273 baseball players with UCL injuries. J Shoulder Elbow Surg 2014;23:1521-6. [Crossref] [PubMed]
- Ahmad CS, Grantham WJ, Greiwe RM. Public perceptions of Tommy John surgery. Phys Sportsmed 2012;40:64-72. [Crossref] [PubMed]
- Conte SA, Hodgins JL, ElAttrache NS, et al. Media perceptions of Tommy John surgery. Phys Sportsmed 2015;43:375-80. [Crossref] [PubMed]
- Rettig AC, Sherrill C, Snead DS, et al. Nonoperative treatment of ulnar collateral ligament injuries in throwing athletes. Am J Sports Med 2001;29:15-7. [Crossref] [PubMed]
- Petty DH, Andrews JR, Fleisig GS, et al. Ulnar collateral ligament reconstruction in high school baseball players: clinical results and injury risk factors. Am J Sports Med 2004;32:1158-64. [Crossref] [PubMed]
- Jones KJ, Dines JS, Rebolledo BJ, et al. Operative management of ulnar collateral ligament insufficiency in adolescent athletes. Am J Sports Med 2014;42:117-21. [Crossref] [PubMed]
- Salvo JP, Rizio L 3rd, Zvijac JE, et al. Avulsion fracture of the ulnar sublime tubercle in overhead throwing athletes. Am J Sports Med 2002;30:426-31. [Crossref] [PubMed]
- Caliandro P, La Torre G, Padua R, et al. Treatment for ulnar neuropathy at the elbow. Cochrane Database Syst Rev 2016;11:CD006839 [PubMed]
- Glajchen N, Schwartz ML, Andrews JR, et al. Avulsion fracture of the sublime tubercle of the ulna: a newly recognized injury in the throwing athlete. AJR Am J Roentgenol 1998;170:627-8. [Crossref] [PubMed]
- Savoie FH 3rd, Trenhaile SW, Roberts J, et al. Primary repair of ulnar collateral ligament injuries of the elbow in young athletes: a case series of injuries to the proximal and distal ends of the ligament. Am J Sports Med 2008;36:1066-72. [Crossref] [PubMed]
- Podesta L, Crow SA, Volkmer D, et al. Treatment of partial ulnar collateral ligament tears in the elbow with platelet-rich plasma. Am J Sports Med 2013;41:1689-94. [Crossref] [PubMed]
- Hurwit DJ, Garcia GH, Liu J, et al. Management of ulnar collateral ligament injury in throwing athletes: a survey of the American Shoulder and Elbow Surgeons. J Shoulder Elbow Surg 2017;26:2023-8. [Crossref] [PubMed]
- Hunter LY, O'Connor GA. Traction apophysitis of the olecranon. A case report. Am J Sports Med 1980;8:51-2. [Crossref] [PubMed]
- Ahmad CS, ElAttrache NS. Valgus extension overload syndrome and stress injury of the olecranon. Clin Sports Med 2004;23:665-76. x. [Crossref] [PubMed]
- Matsuura T, Kashiwaguchi S, Iwase T, et al. The value of using radiographic criteria for the treatment of persistent symptomatic olecranon physis in adolescent throwing athletes. Am J Sports Med 2010;38:141-5. [Crossref] [PubMed]
- Schickendantz MS, Ho CP, Koh J. Stress injury of the proximal ulna in professional baseball players. Am J Sports Med 2002;30:737-41. [Crossref] [PubMed]
- Rettig AC, Wurth TR, Mieling P. Nonunion of olecranon stress fractures in adolescent baseball pitchers: a case series of 5 athletes. Am J Sports Med 2006;34:653-6. [PubMed]
- Paci JM, Dugas JR, Guy JA, et al. Cannulated screw fixation of refractory olecranon stress fractures with and without associated injuries allows a return to baseball. Am J Sports Med 2013;41:306-12. [Crossref] [PubMed]
- Singer KM, Roy SP. Osteochondrosis of the humeral capitellum. Am J Sports Med 1984;12:351-60. [Crossref] [PubMed]
- Kobayashi K, Burton KJ, Rodner C, et al. Lateral compression injuries in the pediatric elbow: Panner's disease and osteochondritis dissecans of the capitellum. J Am Acad Orthop Surg 2004;12:246-54. [Crossref] [PubMed]
- Hsu SH, Moen TC, Levine WN, et al. Physical examination of the athlete's elbow. Am J Sports Med 2012;40:699-708. [Crossref] [PubMed]
- Baumgarten TE, Andrews JR, Satterwhite YE. The arthroscopic classification and treatment of osteochondritis dissecans of the capitellum. Am J Sports Med 1998;26:520-3. [Crossref] [PubMed]
- Matsuura T, Kashiwaguchi S, Iwase T, et al. Conservative treatment for osteochondrosis of the humeral capitellum. Am J Sports Med 2008;36:868-72. [Crossref] [PubMed]
- Takahara M, Shundo M, Kondo M, et al. Early detection of osteochondritis dissecans of the capitellum in young baseball players. Report of three cases. J Bone Joint Surg Am 1998;80:892-7. [Crossref] [PubMed]
- Bradley JP, Petrie RS. Osteochondritis dissecans of the humeral capitellum. Diagnosis and treatment. Clin Sports Med 2001;20:565-90. [Crossref] [PubMed]
- Dwek JR. A segmental approach to imaging of sports-related injuries of the pediatric elbow. Sports Health 2012;4:442-52. [Crossref] [PubMed]
- Kramer D. Elbow pain and injury in young athletes. J Pediatr Orthop 2011;20:S7-12.
- Haraldsson S. On osteochondrosis deformas juvenilis capituli humeri including investigation of intra-osseus vasculature in distal humerus. Acta Orthop Scand Suppl 1959;38:1-232. [PubMed]
- Ahmad CS, Vitale MA, ElAttrache NS. Elbow arthroscopy: capitellar osteochondritis dissecans and radiocapitellar plica. Instr Course Lect 2011;60:181-90. [PubMed]
- Mihara K, Tsutsui H, Nishinaka N, et al. Nonoperative treatment for osteochondritis dissecans of the capitellum. Am J Sports Med 2009;37:298-304. [Crossref] [PubMed]
- Arai Y, Hara K, Fujiwara H, et al. A new arthroscopic-assisted drilling method through the radius in a distal-to-proximal direction for osteochondritis dissecans of the elbow. Arthroscopy 2008;24:237.e1-4. [Crossref] [PubMed]
- Takahara M, Ogino T, Sasaki I, et al. Long term outcome of osteochondritis dissecans of the humeral capitellum. Clin Orthop Relat Res 1999;108-15. [PubMed]
- Ruch DS, Cory JW, Poehling GG. The arthroscopic management of osteochondritis dissecans of the adolescent elbow. Arthroscopy 1998;14:797-803. [Crossref] [PubMed]
- Krijnen MR, Lim L, Willems WJ. Arthroscopic treatment of osteochondritis dissecans of the capitellum: Report of 5 female athletes. Arthroscopy 2003;19:210-4. [Crossref] [PubMed]
- Byrd JW, Jones KS. Arthroscopic surgery for isolated capitellar osteochondritis dissecans in adolescent baseball players: minimum three-year follow-up. Am J Sports Med 2002;30:474-8. [Crossref] [PubMed]
- Nobuta S, Ogawa K, Sato K, et al. Clinical outcome of fragment fixation for osteochondritis dissecans of the elbow. Ups J Med Sci 2008;113:201-8. [Crossref] [PubMed]
- Harada M, Ogino T, Takahara M, et al. Fragment fixation with a bone graft and dynamic staples for osteochondritis dissecans of the humeral capitellum. J Shoulder Elbow Surg 2002;11:368-72. [Crossref] [PubMed]
- Takeda H, Watarai K, Matsushita T, et al. A surgical treatment for unstable osteochondritis dissecans lesions of the humeral capitellum in adolescent baseball players. Am J Sports Med 2002;30:713-7. [Crossref] [PubMed]
- Iwasaki N, Kato H, Ishikawa J, et al. Autologous osteochondral mosaicplasty for capitellar osteochondritis dissecans in teenaged patients. Am J Sports Med 2006;34:1233-9. [Crossref] [PubMed]
- Ansah P, Vogt S, Ueblacker P, et al. Osteochondral transplantation to treat osteochondral lesions in the elbow. J Bone Joint Surg Am 2007;89:2188-94. [PubMed]
- Fleisig GS, Andrews JR, Cutter GR, et al. Risk of serious injury for young baseball pitchers: a 10-year prospective study. Am J Sports Med 2011;39:253-7. [Crossref] [PubMed]
- Lyman S, Fleisig GS, Andrews JR, et al. Effect of pitch type, pitch count, and pitching mechanics on risk of elbow and shoulder pain in youth baseball pitchers. Am J Sports Med 2002;30:463-8. [Crossref] [PubMed]
- Guidelines for Youth and Adolescent Pitchers. Available online: http://m.mlb.com/pitchsmart/pitching-guidelines/. Accessed October 10, 2017.
- Regular Season Pitching Rules - Baseball. Available online: http://www.littleleague.org/assets/forms_pubs/media/pitchingregulationchanges_bb_11-13-09.pdf. Accessed October 10, 2017.
- Limpisvasti O, ElAttrache NS, Jobe FW. Understanding shoulder and elbow injuries in baseball. J Am Acad Orthop Surg 2007;15:139-47. [Crossref] [PubMed]
- Kibler WB, Press J, Sciascia A. The role of core stability in athletic function. Sports Med 2006;36:189-98. [Crossref] [PubMed]
- Ellenbecker TS, Reinold M, Nelson CO. Clinical concepts for treatment of the elbow in the adolescent overhead athlete. Clin Sports Med 2010;29:705-24. [Crossref] [PubMed]
Cite this article as: Andelman S, DiPrinzio E, Hausman M. Elbow injuries in the pediatric athlete. Ann Joint 2018;3:21.


